
The Tech Maverick: Ivan Teh’s Impact On Fusionex’s Success Story
Imagine a world where technology has the power to transform businesses, revolutionize industries, and empower individuals to reach new heights of success. In this digital era, one name stands out as a true maverick in the tech industry – Ivan Teh. With his visionary leadership and relentless pursuit of innovation, Teh has played a pivotal role in shaping the remarkable success story of Fusionex, a leading big data analytics company. From revolutionizing the way businesses harness the power of data to pioneering groundbreaking technologies, Teh’s impact has been nothing short of extraordinary. Join us as we explore the fascinating journey of this tech maverick and discover how his brilliance has paved the way for Fusionex’s unparalleled achievements.
The Tech Maverick: Ivan Teh’s Impact on Fusionex’s Success Story

Background of Fusionex
Brief overview of Fusionex
Fusionex is a leading tech company that specializes in big data analytics, artificial intelligence, and machine learning. Established in 2006, Fusionex has quickly gained recognition and credibility for its innovative solutions and cutting-edge technologies. With a strong focus on harnessing the power of data, the company has successfully transformed businesses across various industries.
Introduction of Ivan Teh
At the heart of Fusionex’s success is Ivan Teh, the visionary leader who co-founded the company and serves as its Chief Executive Officer. With his relentless drive and passion for technology, Teh has steered Fusionex to new heights, establishing it as a prominent player in the tech industry. Known for his forward-thinking approach and commitment to innovation, Teh’s leadership has been instrumental in shaping Fusionex’s growth and success.
Early Days and Founding of Fusionex
The inception of Fusionex
Fusionex was founded in 2006 with the aim of revolutionizing the way businesses leverage data for strategic decision-making. Teh, along with a group of like-minded individuals, saw the immense potential of data analytics and believed in its ability to drive business growth and success. With this vision in mind, Fusionex was born.
Ivan Teh’s role in starting the company
As one of the co-founders, Ivan Teh played a pivotal role in the establishment of Fusionex. With his expertise in technology and his passion for innovation, Teh contributed significantly to the development of Fusionex’s core offerings and solutions. His ability to envision the possibilities of big data analytics and his determination to make it a reality were instrumental in shaping the company’s direction and mission.
Challenges faced in the early days
Like any startup, Fusionex faced its fair share of challenges in its early days. The tech industry was highly competitive, and convincing businesses to embrace the power of data analytics was no easy feat. However, Teh’s unwavering belief in the transformative potential of their solutions propelled Fusionex forward. With a customer-centric approach and a relentless pursuit of excellence, Fusionex overcame these challenges and solidified its position as a key player in the tech industry.
Fusionex’s Growth and Expansion
Successful projects and partnerships
Over the years, Fusionex has undertaken numerous successful projects and established key partnerships with leading industry players. Through its innovative solutions, the company has helped businesses across various sectors unlock the full potential of their data and achieve remarkable results. Fusionex’s ability to deliver tangible outcomes has earned it a reputation as a trusted partner in the industry.
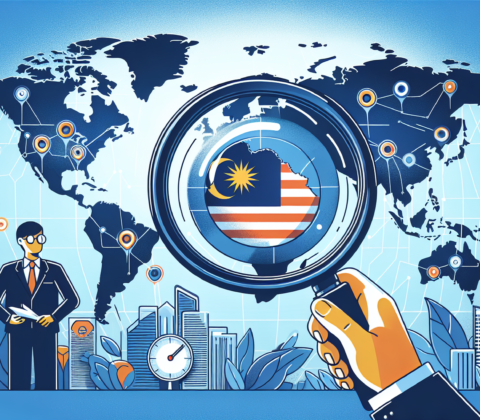
Expansion into new markets
As Fusionex’s reputation grew, so did its reach. The company expanded into new markets, both domestically and internationally, to cater to the increasing demand for its services. With a strong presence in Asia, Europe, and the United States, Fusionex is well-positioned to serve a diverse range of clients and industries.
Fusionex’s positioning in the tech industry
Today, Fusionex is widely recognized as a leading player in the tech industry, particularly in the field of big data analytics. Its innovative solutions have disrupted traditional business models and provided businesses with the tools they need to thrive in the digital age. Fusionex’s commitment to excellence and continuous innovation has solidified its position as a trailblazer in the industry.
Ivan Teh’s Leadership Style
Influences and inspirations
Ivan Teh’s leadership style is a testament to his passion for innovation and technology. Influenced by visionaries such as Steve Jobs and Elon Musk, Teh believes in pushing boundaries and challenging the status quo. His relentless pursuit of excellence and his ability to think outside the box have set him apart as a leader in the tech industry.
Approach to innovation and technology
Teh’s approach to innovation and technology is centered around the idea of constant evolution. He believes that technology should never be stagnant and that businesses should continuously adapt to stay ahead of the curve. Teh fosters a culture of innovation within Fusionex, encouraging employees to embrace new technologies and explore creative solutions to solve complex problems.
Creating a positive work culture
As a leader, Teh understands the importance of creating a positive work culture that fosters creativity and collaboration. At Fusionex, employees are encouraged to think freely, share ideas, and learn from one another. Teh believes that a strong team is the foundation of any successful company and strives to create an inclusive and supportive environment where everyone can thrive.
Innovative Solutions Introduced by Fusionex
Overview of Fusionex’s flagship products
Fusionex has introduced a range of innovative solutions that leverage the power of big data analytics. From its flagship product, Fusionex GIANT, to its advanced AI and machine learning capabilities, the company offers a comprehensive suite of tools to help businesses make data-driven decisions. Fusionex’s solutions are designed to be scalable, user-friendly, and customizable to meet the unique needs of each client.
Impacts of these solutions on industries
Fusionex’s solutions have had a profound impact on industries across the board. By harnessing the power of data, businesses have been able to gain valuable insights, optimize operations, and drive revenue growth. From healthcare and finance to manufacturing and retail, Fusionex’s solutions have transformed the way businesses operate, giving them a competitive edge in the digital age.
Successful case studies
Fusionex’s success can be seen through numerous case studies that highlight the transformative power of its solutions. For example, in the healthcare industry, Fusionex’s data analytics platform has helped hospitals improve patient outcomes by identifying patterns and predicting disease progression. In the retail sector, its advanced analytics tools have enabled businesses to better understand customer behavior and tailor marketing campaigns for maximum impact. These success stories showcase the real-world applications of Fusionex’s innovative solutions.
Collaborations and Partnerships
Key partnerships established by Fusionex
Fusionex has forged strategic partnerships with industry leaders to further enhance its offerings and expand its reach. These partnerships have allowed Fusionex to tap into new markets, leverage complementary expertise, and deliver even greater value to its clients. By collaborating with other tech companies, Fusionex has been able to stay at the forefront of technological advancements and continuously innovate its solutions.
Collaborative projects with other tech companies
In addition to partnerships, Fusionex has also embarked on collaborative projects with other tech companies to address complex challenges and drive innovation. By combining resources and expertise, these collaborations have resulted in groundbreaking solutions that push the boundaries of what is possible in the tech industry. Fusionex’s ability to foster collaboration and build strong relationships within the industry has been instrumental in its success.
Recognition and Awards
Notable industry recognitions received by Fusionex
Fusionex’s commitment to excellence and innovation has been recognized by the industry, earning the company numerous accolades. These recognitions serve as a testament to Fusionex’s impact on the tech industry and its ability to deliver tangible results. Awards such as the Big Data Analytics Excellence Award and the AI Innovation Award further solidify Fusionex’s position as a trailblazer in the field.
Individual accolades for Ivan Teh
As the driving force behind Fusionex, Ivan Teh has also received individual accolades for his contributions to the industry. He has been recognized as a tech maverick and a thought leader, inspiring others with his passion and dedication to technology. Teh’s visionary leadership and his ability to translate ideas into reality have earned him a reputation as one of the industry’s most influential figures.
Challenges Overcome and Lessons Learned
Obstacles faced by Fusionex
Throughout its journey, Fusionex has faced its fair share of obstacles and setbacks. From the early days of convincing businesses to embrace data analytics to navigating the challenges of scaling operations, the company has encountered numerous hurdles along the way. However, Fusionex’s resilience and commitment to its mission have allowed it to overcome these obstacles and emerge stronger.
How Ivan Teh led the company through challenges
As a leader, Ivan Teh has played a crucial role in guiding Fusionex through its challenges. His strategic vision, unwavering determination, and ability to inspire others have been instrumental in overcoming obstacles. Teh’s hands-on approach and willingness to roll up his sleeves have created a culture of resilience within Fusionex, motivating employees to tackle challenges head-on and find innovative solutions.
Lessons learned from setbacks
Fusionex’s journey has taught the company and its leaders valuable lessons that have shaped its continued success. From setbacks, they have learned the importance of adaptability, agility, and perseverance. Fusionex embraces failure as an opportunity for growth and strives to continuously iterate and improve its offerings. These lessons have not only strengthened the company but also positioned it for future success.
Impact on the Big Data Analytics Industry
Introduction of big data analytics
Big data analytics refers to the process of extracting actionable insights from large and complex datasets. It is a rapidly growing field that has become essential for businesses looking to gain a competitive advantage. By leveraging advanced analytics techniques, businesses can uncover hidden patterns, trends, and correlations within their data, enabling them to make informed and data-driven decisions.
Fusionex’s contributions to the field
Fusionex has made significant contributions to the big data analytics industry through its innovative solutions and pioneering technologies. By developing user-friendly and scalable analytics tools, Fusionex has made it easier for businesses to harness the power of data and derive meaningful insights. Its advanced algorithms and machine learning capabilities have helped businesses uncover valuable insights that were previously hidden in their data.
How Ivan Teh’s vision shaped the industry
Ivan Teh’s vision and leadership have played a pivotal role in shaping the big data analytics industry. By championing the importance of data-driven decision-making, Teh has inspired businesses to embrace the power of data analytics and explore its transformative potential. His commitment to innovation and his relentless pursuit of excellence have set a new standard for the industry, pushing businesses to continuously evolve and adapt to the digital age.
Future Outlook and Strategy
Fusionex’s vision for the future
Looking ahead, Fusionex’s vision is to continue pioneering innovative solutions that empower businesses to harness the full potential of their data. The company aims to be at the forefront of technological advancements, constantly pushing the boundaries of what is possible. Fusionex envisions a future where data analytics becomes an integral part of every business, enabling them to thrive in an increasingly data-driven world.
Expansion plans and goals
As part of its growth strategy, Fusionex plans to expand its presence in new markets and industries. The company seeks to forge new partnerships and collaborations to further enhance its offerings and deliver even greater value to its clients. Fusionex aims to be the go-to provider for big data analytics and continue to revolutionize the way businesses leverage data for strategic decision-making.
Ivan Teh’s role in driving future success
Ivan Teh will continue to play a pivotal role in driving Fusionex’s future success. As the visionary leader, Teh will guide the company’s strategic direction, ensuring that Fusionex remains at the forefront of innovation and technology. His passion for technology, his commitment to excellence, and his ability to inspire others will be invaluable in shaping Fusionex’s future and cementing its position as a leader in the tech industry.
As Fusionex continues to disrupt the tech industry and transform businesses with its innovative solutions, Ivan Teh’s impact on the company’s success story cannot be overstated. Through his visionary leadership, relentless pursuit of excellence, and commitment to innovation, Teh has propelled Fusionex to new heights, solidifying its position as a trailblazer in the field of big data analytics. With Teh at the helm, Fusionex’s future looks bright as it continues to shape the way businesses leverage data to drive growth, efficiency, and success in the digital age.

How To Choose The Best SEO Service In Malaysia For Your Business
Are you searching for the best SEO service in Malaysia to boost your business? Look no further! In this article, we will guide you through the process of choosing the perfect SEO service provider for your specific needs. Whether you’re a small startup or a well-established company, we understand the importance of reaching your target audience and improving your online presence. With our friendly and comprehensive approach, we’ll walk you through the steps so you can make an informed decision and take your business to new heights. Let’s get started!
Choosing the Right SEO Service in Malaysia
Are you a business owner in Malaysia looking to improve your online visibility and attract more customers? If so, choosing the right SEO service is essential. Search Engine Optimization (SEO) plays a crucial role in driving organic web traffic, increasing brand awareness, and ultimately, boosting sales. With so many SEO service providers available in the market, it can be overwhelming to make the right choice. But fear not, this comprehensive article will guide you through the process of selecting the best SEO service in Malaysia for your business.
Understanding the Importance of SEO for Your Business
Before diving into the process of selecting an SEO service provider, let’s first understand the importance of SEO for your business. SEO is the practice of optimizing your website to rank higher in search engine results pages (SERPs). By improving your website’s visibility, you can attract more organic (unpaid) traffic and increase your chances of converting visitors into customers.
The basics of SEO involve various strategies and techniques such as keyword research, on-page optimization, link building, and content creation. A well-executed SEO strategy can bring numerous benefits to your business, including increased website traffic, improved brand visibility, enhanced user experience, and higher search engine rankings.
Determining Your SEO Goals and Objectives
Before embarking on your search for an SEO service provider, it’s crucial to determine your SEO goals and objectives. Identifying what you want to achieve through SEO will help you find the right service provider who aligns with your business needs.
Start by identifying your target audience and market. Understanding who your potential customers are and where they are located will give you insights into the SEO strategies required to reach them effectively.
Next, define your Key Performance Indicators (KPIs). These are measurable metrics that will help gauge the success of your SEO efforts. Whether it’s increasing website traffic, improving search engine rankings, or generating more leads, establishing clear KPIs will allow you to track progress and evaluate the effectiveness of the SEO service provider.
Lastly, set realistic SEO goals for your business. Ensure that your goals are attainable within a reasonable timeframe and align with your overall business objectives. Clear goals will also provide a benchmark for evaluating the performance of the SEO service provider.

Researching and Shortlisting SEO Service Providers
With your SEO goals in mind, it’s time to conduct thorough research and shortlist potential SEO service providers. Start by performing an online search, focusing on companies that specialize in SEO services and have a strong presence in Malaysia. You can use search engines, business directories, and industry-specific websites to find potential candidates.
Reading reviews and testimonials is an excellent way to gauge the reputation and credibility of SEO service providers. Look for feedback from their previous clients to get insights into their service quality, customer satisfaction, and results achieved. Positive reviews and testimonials can instill confidence in their ability to deliver effective SEO solutions for your business.
Furthermore, check for accreditations and certifications. A reputable SEO service provider should have certifications from recognized organizations such as Google, Bing, or SEMrush. These certifications validate their expertise and commitment to staying updated with the latest SEO practices.
Assessing the Reputation and Experience of SEO Service Providers
Once you have shortlisted a few SEO service providers, it’s essential to assess their reputation and experience. Start by evaluating their website and online presence. A professionally designed and optimized website indicates their knowledge and expertise in the field. Look for case studies, client success stories, and industry awards that can further establish their credibility.
Client testimonials play a vital role in determining the trustworthiness of SEO service providers. Reach out to their past or existing clients if possible to gather more information about their experiences. A reliable SEO service provider will have a proven track record of delivering results and building long-term relationships with clients.

Analyzing the SEO Service Provider’s Track Record and Case Studies
To gain deeper insights into the performance of SEO service providers, it’s crucial to evaluate their track record and case studies. Assess their past projects and results to determine if they have experience in your industry or niche. A service provider with relevant experience will have a better understanding of your business needs and can tailor their strategies accordingly.
Verifying the authenticity of case studies is critical. Look for tangible results achieved by the SEO service provider, such as improved search rankings, increased organic traffic, or higher conversion rates. Ideally, seek case studies that showcase long-term success to ensure the service provider consistently delivers results.
Furthermore, consider the longevity of their client relationships. A service provider with long-term clients suggests their ability to maintain client satisfaction and provide ongoing support. Long-lasting partnerships indicate a high level of trust and reliability.
Considering the Range of SEO Services Offered
The range of SEO services offered by a service provider is another crucial factor to consider. An effective SEO strategy encompasses various aspects, including on-page optimization, off-page SEO strategies, technical SEO capabilities, and local SEO expertise.
On-page SEO optimization focuses on optimizing individual web pages to improve their search engine rankings. It involves optimizing meta tags, headings, content, and URL structure. Be sure to choose a service provider that excels in this area to ensure your website performs well in search engine results.
Off-page SEO strategies involve building high-quality backlinks and enhancing your website’s online reputation. A reliable SEO service provider will have effective strategies for acquiring backlinks from reputable websites, which can improve your website’s authority and visibility.
Technical SEO capabilities are crucial for ensuring your website is crawlable and accessible by search engine bots. This includes optimizing website speed, mobile-friendliness, and site architecture. Choose an SEO service provider that has expertise in technical SEO to improve your website’s overall performance.
Local SEO expertise is especially important for businesses targeting a specific geographical area. The service provider should be knowledgeable in optimizing your website for local search results, including Google My Business optimization, local citations, and customer reviews.
Evaluating the Expertise and Skill Set of the SEO Team
The expertise and skill set of the SEO team working for the service provider should not be overlooked. A competent SEO team will have the knowledge and experience to implement effective strategies that align with your business goals.
Understand the qualifications and background of the SEO team. Look for team members with relevant certifications and training from reputable organizations in the field of SEO. This ensures they possess the necessary skills and expertise to handle your SEO needs.
Additionally, assess their experience with similar businesses or industries. An SEO team with experience in your particular niche will have a better understanding of the challenges and opportunities your business faces. Their industry knowledge can result in more tailored and effective SEO strategies.
Examining the SEO Service Provider’s Communication and Reporting
Effective communication and transparent reporting are vital for a successful partnership with an SEO service provider. Evaluate the communication channels they offer and their response time. Choose a provider that offers regular updates and prompt communication to address any concerns or questions you may have.
Understanding the SEO reporting structure and frequency is crucial. The service provider should provide comprehensive reports that outline the progress of your SEO campaigns and the results achieved. Clear and transparent reporting allows you to track the effectiveness of their strategies and make informed decisions.
Determine the availability of account managers. Having a dedicated account manager can ensure personalized attention to your needs and prompt resolution of any issues that may arise. The account manager acts as the point of contact between you and the SEO service provider, facilitating effective communication and collaboration.
Reviewing the Pricing and Contract Terms
When considering SEO service providers, reviewing the pricing and contract terms is essential. Request detailed pricing information from the shortlisted providers and compare them to ensure you are getting value for your investment. Be cautious of extremely low-priced services, as they may indicate a lack of expertise or a shortcut approach that could harm your website’s search engine rankings.
Carefully review the contract terms before making a decision. Understand the duration of the contract, cancellation policies, and any additional costs or hidden fees. A reputable SEO service provider will be transparent about their pricing structure and contract terms, ensuring you can make an informed decision.
Seeking Recommendations and Referrals
Lastly, seeking recommendations and referrals can provide valuable insights when choosing an SEO service provider. Ask for referrals from trusted sources such as friends, business associates, or industry peers who have experience with SEO services. Their firsthand recommendations can help you identify reliable providers and narrow down your choices.
Additionally, consult online SEO communities and forums to gather more information about SEO service providers in Malaysia. These communities are a great resource for insights, feedback, and experiences shared by SEO professionals and businesses alike. Engaging in discussions can help you gain a better understanding of the reputable SEO service providers in the market.
By following these guidelines and thoroughly evaluating potential SEO service providers, you can make an informed decision that aligns with your business goals. Remember, selecting the right SEO service provider is an investment in the growth and success of your business in the digital landscape.


Fusionex’s Financial Crisis Deepens: Winding Up And Bankruptcy Looming
Hey there! Have you heard the news about Fusionex’s financial crisis? It seems like things are getting pretty intense, with the possibility of winding up and bankruptcy looming over them. In this article, we’ll delve into the details of what’s going on and explore how this could potentially impact the future of the company. Buckle up and get ready to dive into the world of big data and business struggles. Trust me, this is an article you won’t want to miss!

Overview of Fusionex’s Financial Crisis
Introduction to Fusionex
Fusionex is a prominent player in the big data industry, known for its innovative solutions and advanced analytics capabilities. The company has carved a niche for itself by providing businesses with valuable insights that enhance decision-making. With a strong track record of delivering cutting-edge solutions, Fusionex quickly gained popularity and established a robust presence in the market.
Emerging Financial Crisis
However, in recent times, Fusionex has been facing an increasingly deepening financial crisis. The once thriving company has found itself grappling with a range of challenges that have put its stability and future at risk. This crisis has not only stressed the organization but has also raised concerns among stakeholders and industry observers.
Current State of Affairs
At present, Fusionex finds itself in a dire situation as it contemplates winding up and potential bankruptcy. The financial turmoil has cast a dark cloud over the company’s future and has left employees, creditors, and investors uncertain about what lies ahead. The next sections will delve into the factors that have contributed to this crisis and the implications it holds for Fusionex and its stakeholders.
Factors Contributing to the Crisis
Mismanagement and Poor Governance
Mismanagement and poor governance have played a significant role in Fusionex’s financial downfall. Ineffective decision-making processes, lack of proper oversight, and questionable practices have undermined the company’s financial health. These factors have eroded investor confidence and have added to the mounting challenges faced by Fusionex.
Decline in Financial Performance
Fusionex has experienced a notable decline in its financial performance, which further exacerbates its crisis. The company’s revenue has dwindled, and profitability has taken a hit, raising concerns about its ability to sustain its operations. Poor cost management and failure to adapt swiftly to market dynamics have fueled this decline, putting Fusionex in a precarious position.
Legal and Regulatory Issues
Fusionex has also been entangled in a web of legal and regulatory issues that have strained its resources and reputation. The company has faced lawsuits, fines, and investigations, leading to financial burdens and reputational damage. Navigating through these legal challenges has proven to be a substantial hurdle, adding more weight to Fusionex’s ongoing crisis.
Fusionex’s Winding Up Process
Definition and Purpose of Winding Up
Winding up, also known as liquidation, is a process wherein a company opts to cease its operations and distribute its assets to settle its debts. The purpose of such a process is to bring closure to a financially distressed company and allow for an orderly distribution of its resources among its creditors.
Fusionex’s Decision to Wind Up
Given the gravity of its financial crisis, Fusionex has made the difficult decision to wind up its operations. This decision signifies the seriousness of the company’s predicament and the absence of viable alternatives to salvage the situation. The winding up process is an arduous one, and Fusionex is now faced with navigating through its stages.
Stages in the Winding Up Process
The winding up process consists of several stages, each with its own requirements and implications. Initially, Fusionex will appoint a liquidator who assumes control over the company’s affairs. The liquidator is responsible for identifying and realizing the company’s assets, settling its liabilities, and distributing any remaining funds to creditors. This process may involve investigations, creditor meetings, and the submission of financial reports.
Impact on Employees and Stakeholders
The decision to wind up Fusionex has profound consequences for its employees and stakeholders. Employees may face job insecurity and the possibility of layoffs as the company seeks to streamline its operations. Stakeholders, including suppliers and investors, may also suffer losses as the winding up process unfolds. These challenges highlight the far-reaching effects of Fusionex’s financial crisis on its ecosystem.

Legal Implications and Challenges
Role of Liquidators
Liquidators play a critical role in the winding up process, tasked with managing the affairs of the distressed company. They are responsible for preserving and liquidating the company’s assets, investigating its financial affairs, and facilitating the orderly distribution of funds to creditors. The appointment of a competent and impartial liquidator can significantly impact the outcome of the process.
Creditors’ Rights and Claims
During the winding up process, creditors have the right to submit their claims and seek repayment from the company. The liquidator diligently examines these claims, verifying their validity and determining the priority of payment. Creditors may need to provide evidence to support their claims, ensuring a fair and equitable distribution of assets.
Liquidation of Assets
Liquidating assets is a critical step in the winding up process. Fusionex’s assets, which may include intellectual property, technology, and physical property, need to be efficiently and fairly converted into cash to satisfy the company’s debts. The liquidation process requires careful evaluation, valuation, and sale of these assets to maximize their value.
Potential Disputes and Litigation
The winding up process may give rise to disputes and litigation, particularly when stakeholders contest the distribution of assets or challenge decisions made by the liquidator. These legal battles can delay the resolution of the crisis, prolong proceedings, and increase costs. Resolving such disputes in a timely and just manner is essential for the successful completion of Fusionex’s winding up process.
Bankruptcy Proceedings and Consequences
Bankruptcy Defined
Bankruptcy is a legal process initiated by a debtor who is unable to repay their debts. It offers a framework for the restructuring or liquidation of a company’s assets to satisfy its financial obligations. Bankruptcy proceedings can be voluntary, initiated by the company itself, or involuntary, instigated by creditors seeking recourse.
Initiating Bankruptcy Proceedings
While Fusionex has decided to wind up, it may still face the possibility of bankruptcy proceedings if it fails to satisfy its debts through the winding up process. The decision to initiate bankruptcy proceedings can be made by either the company or its creditors, depending on the circumstances. These proceedings would provide a more structured approach to resolving Fusionex’s financial crisis.
Effects on Fusionex and its Reputation
Bankruptcy can have severe consequences for Fusionex, impacting its operations, reputation, and market standing. Suppliers and customers may lose confidence in the company’s ability to fulfill its obligations, leading to a decline in business opportunities. Rebuilding its reputation following bankruptcy can prove to be a substantial undertaking, requiring steady and strategic efforts.
Impacts on Creditors and Investors
Bankruptcy proceedings would have significant implications for Fusionex’s creditors and investors. Creditors, depending on the priority of their claims, may face the prospect of receiving only a fraction of what they are owed. Investors, particularly shareholders, may witness a significant depreciation in the value of their investment. These consequences further underscore the urgency of addressing the financial crisis and exploring potential solutions.
Attempts at Financial Restructuring
Negotiations with Creditors
As Fusionex grapples with its financial crisis, negotiations with creditors can provide a potential avenue for resolving outstanding debt. Collaborative discussions may lead to debt restructuring, repayment plans, or the modification of terms to alleviate the burden on the company. Open lines of communication and a willingness to find mutually beneficial solutions are critical during this process.
Debt Restructuring Options
Debt restructuring refers to modifying the terms of existing debt to enhance its viability and improve the company’s financial situation. This may involve reducing interest rates, extending repayment periods, or converting debt into equity. Debt restructuring options can offer a lifeline to Fusionex, allowing it to reestablish its financial footing and restore confidence among stakeholders.
Possibilities for Resolving the Crisis
While the financial crisis may seem daunting, there are possibilities for resolving the challenges faced by Fusionex. By actively engaging in negotiations, exploring debt restructuring options, and reviewing the company’s operations, Fusionex can identify potential strategies to navigate its way out of the crisis. These actions require careful analysis, collaboration, and a willingness to adapt.
Market Response and Investor Confidence
Share Price Performance
The financial crisis at Fusionex has inevitably affected the company’s share price. The decline in financial performance, legal issues, and potential winding up or bankruptcy have caused investors to lose confidence, leading to a decrease in share value. The share price performance serves as an indicator of the market’s perception of Fusionex’s current state and its ability to recover.
Analysts’ Views and Recommendations
Financial analysts closely monitor Fusionex and provide insights into the company’s prospects. Their views and recommendations can shed light on Fusionex’s current position and future outlook. Analysts may offer guidance on potential actions the company can take to recover from the crisis, providing valuable perspectives to investors and stakeholders.
Investor Sentiment
Investor sentiment has a considerable impact on Fusionex’s ability to weather the financial storm. Negative sentiment may lead to increased selling pressure, further eroding share prices and hindering the company’s recovery. Conversely, positive sentiment can lay the foundation for renewed confidence, attracting investors who see the potential for a rebound.
Industry and Competitor Analysis
Competitor Performance and Positioning
Analyzing Fusionex’s competitors can provide insights into the broader industry landscape and shed light on how the financial crisis impacts the company’s competitive positioning. Examining competitors’ financial performance, strategies, and market share can help identify opportunities and threats for Fusionex. This analysis is crucial for formulating effective recovery plans and realigning the company’s position in the industry.
Market Trends and Outlook
Understanding market trends is vital to Fusionex’s recovery efforts. Shifting dynamics, emerging technologies, and changing customer demands can significantly impact the company’s future prospects. By monitoring market trends and keeping a pulse on industry developments, Fusionex can adapt, innovate, and position itself for sustainable growth amidst the financial crisis.
Implications for the Big Data Industry
The financial crisis at Fusionex has implications beyond the company itself. As a prominent player in the big data industry, Fusionex’s challenges raise questions about the sector as a whole. Observing how Fusionex and the industry navigate through this crisis provides valuable insights into the resilience and adaptability of the big data industry, shaping its future trajectory.
Impact on Fusionex Employees
Job Security and Layoffs
The financial crisis at Fusionex inevitably creates concerns about job security among its employees. Layoffs may become a painful reality as the company seeks to streamline its operations and reduce costs. Employees may face uncertainty and anxiety about their future, necessitating effective communication, support, and potential career transition initiatives.
Employee Morale and Mental Health
A financial crisis can have a significant impact on employee morale and mental health. The stress and uncertainty resulting from the crisis may lead to decreased productivity, increased absenteeism, and higher turnover rates. Supporting employees’ well-being, providing resources for mental health, and fostering a positive work environment are essential during such challenging times.
Implications for the IT Job Market
The financial crisis at Fusionex may have wider implications for the IT job market. As the company grapples with layoffs and potential winding up, employees may enter the job market seeking new opportunities. This influx of skilled IT professionals can impact the talent pool, industry dynamics, and competition for jobs. Stakeholders should be attentive to the changing landscape and potential opportunities for resource allocation.
The Future of Fusionex
Potential Acquisition or Mergers
In the face of a financial crisis, Fusionex may consider various strategies to secure its future. One potential avenue is pursuing acquisitions or mergers with strategic partners. Such collaborations can provide fresh capital, enhanced capabilities, and expanded market reach, offering Fusionex a lifeline to recover and grow.
Survival Strategies
Fusionex must adopt survival strategies to weather the storm and emerge resilient. These strategies may include exploring new markets or customer segments, diversifying service offerings, or optimizing operational efficiency. Adapting to market realities, capitalizing on core competencies, and embracing innovation are crucial factors in Fusionex’s ability to survive and thrive.
Lessons Learned
The financial crisis at Fusionex serves as a valuable lesson for the company and the industry as a whole. Reflection on the causes, consequences, and recovery efforts can yield insights that shape future decision-making. Learning from the crisis, implementing stronger governance practices, and proactively addressing challenges will be instrumental in preventing a recurrence and ensuring long-term success.

Fusionex Group’s Leadership Spotlight: Driving Growth In The Tech Revolution
In the ever-evolving world of technology, Fusionex Group stands at the forefront, driving growth and innovation through their visionary leadership. With a dedicated focus on the tech revolution, Fusionex Group’s leaders are continuously pushing boundaries and redefining industry standards. Through a friendly and captivating approach, this article explores the remarkable journey of Fusionex Group’s leadership and their significant contributions to the tech revolution. From their expert use of AI and the implementation of proper tagging formats to the inclusion of engaging videos and descriptive alt text, this article invites you to dive deep into the world of Fusionex Group and discover the endless possibilities that await in the realm of technology.
Fusionex Group’s Leadership Spotlight: Driving Growth in the Tech Revolution

Introduction to Fusionex Group
Welcome to Fusionex Group’s Leadership Spotlight! In this article, we will delve into the dynamic world of Fusionex Group and explore how their exceptional leadership is driving growth in the ever-evolving tech revolution. As a leader in the technology industry, Fusionex Group has carved out a unique position for itself, leveraging innovative solutions and strategic partnerships to propel growth and create transformative experiences for its stakeholders.
Understanding the Tech Revolution
The tech revolution has reshaped the world as we know it. From artificial intelligence and big data analytics to cloud computing and internet of things (IoT), technology has become an integral part of our daily lives. Fusionex Group understands the immense potential that lies within this revolution and embraces it wholeheartedly. They recognize that harnessing the power of technology is not only vital for survival but also essential for achieving remarkable growth in the fast-paced digital landscape.
The Role of Leadership in Driving Growth
Leadership plays a crucial role in propelling growth within an organization. A strong and visionary leadership team sets the tone, defines the strategic direction, and empowers the workforce to drive innovation and achieve ambitious goals. At Fusionex Group, their leadership team embodies these qualities, constantly pushing the boundaries of what is possible and fostering a culture of excellence.
Fusionex Group’s Pioneering Leadership
At the helm of Fusionex Group is a group of exceptional leaders who have a deep passion for technology and a wealth of experience in the industry. They have successfully steered the company through shifting market landscapes, emerging trends, and disruptive technologies. With their visionary guidance, Fusionex Group has remained at the forefront of the tech revolution, consistently delivering groundbreaking solutions to meet the evolving needs of their clients.
Developing Innovative Technologies
Innovation is the lifeblood of any technology-driven organization, and Fusionex Group understands this better than anyone else. Their leadership team places a strong emphasis on research and development, constantly exploring new technologies and investing in cutting-edge solutions. By staying ahead of the curve and developing innovative products and services, Fusionex Group is able to not only stay relevant but also drive growth and create a lasting impact in the industry.
Empowering Employees for Success
A successful organization is built on the collective efforts of its employees, and Fusionex Group recognizes the importance of empowering their workforce. Through comprehensive training programs, mentorship initiatives, and a supportive work environment, Fusionex Group enables its employees to reach their full potential. By nurturing talent and fostering a culture of collaboration and innovation, Fusionex Group lays the foundation for sustainable growth and sets themselves apart as an employer of choice in the industry.
Effective Communication Strategies
Communication is key in any organization, and Fusionex Group’s leadership understands the value of effective communication. They ensure that information flows freely across all levels of the organization, keeping everyone aligned with the company’s goals and objectives. By fostering an open and transparent communication culture, Fusionex Group promotes collaboration, encourages feedback, and enables the entire organization to work towards a common vision.
Fostering a Collaborative Work Environment
Collaboration is the fuel that drives innovation, and Fusionex Group thrives on collaboration. The leadership team actively promotes a collaborative work environment, encouraging cross-functional teams to work together and pool their collective expertise. This collaborative approach allows Fusionex Group to leverage diverse perspectives, challenge the status quo, and deliver cutting-edge solutions that address complex business challenges.
Investment in Research and Development
Innovation thrives on research and development, and Fusionex Group recognizes the importance of investing in R&D. Their leadership team allocates significant resources towards research and development, ensuring that they stay at the forefront of technological advancements. By constantly pushing the boundaries of what is possible through R&D, Fusionex Group is able to develop groundbreaking solutions that drive growth and provide a competitive edge in the tech revolution.
Partnerships and Collaborations
Collaboration extends beyond the boundaries of an organization, and Fusionex Group actively seeks partnerships and collaborations with industry leaders, startups, and academia. By forging strategic alliances and leveraging the collective knowledge and expertise of their partners, Fusionex Group is able to accelerate innovation and drive growth. These partnerships allow Fusionex Group to tap into new markets, expand their reach, and deliver transformative solutions to a wider audience.
Conclusion
In conclusion, Fusionex Group’s leadership plays a pivotal role in driving growth in the tech revolution. Through their pioneering vision, dedication to innovation, and commitment to empowering their workforce, Fusionex Group continues to push the boundaries of what is possible in the technology industry. With their strategic partnerships and investments in research and development, they are well-positioned to shape the future of technology and create transformative experiences for their stakeholders. Fusionex Group is undoubtedly a trailblazer in the tech revolution, and their leadership spotlight serves as an inspiration for organizations aspiring to make a lasting impact in the digital landscape.


Tech Trailblazer: The Entrepreneurial Journey Of Ivan Teh And Fusionex
Join us on a captivating journey as we explore the entrepreneurial path of Ivan Teh and the innovative company, Fusionex. In this article, we will delve into the story of a tech trailblazer, highlighting the successes, challenges, and breakthroughs that have shaped their journey. Discover how Teh’s visionary leadership and Fusionex’s cutting-edge solutions have revolutionized the tech industry, and get inspired by their relentless pursuit of excellence. So, buckle up and get ready to be amazed by the entrepreneurial journey of Ivan Teh and Fusionex!
The Early Years: Ivan Teh’s Passion for Technology
Embracing the Digital World
In the fast-paced and ever-evolving landscape of technology, Ivan Teh stands out as a visionary leader. From his early years, it was evident that Teh had a deep passion for all things tech-related. Growing up in a society that was just beginning to embrace the digital world, he quickly recognized the immense potential technology held for transforming industries, improving lives, and driving progress.
Nurturing a Passion
Teh’s journey into the realm of technology began with a fascination for computers and software. As a young child, he would spend hours tinkering with computers, seeking to understand their inner workings and exploring their capabilities. This passion only grew stronger as he entered his teenage years, leading him to pursue formal education in the field of computer science.
From Vision to Reality: The Birth of Fusionex
A Vision Takes Shape
While still in the early stages of his career, Teh had a grand vision – to harness the power of data to drive meaningful insights and create groundbreaking solutions for businesses worldwide. With this vision in mind, he founded Fusionex in 2006, setting the stage for a remarkable entrepreneurial journey.
Fostering Innovation
Fusionex quickly gained recognition as a leading provider of enterprise data solutions and analytics. From the very beginning, Teh’s relentless drive for innovation and his unwavering commitment to excellence laid the foundation for the company’s success. Under his leadership, Fusionex embarked on a mission to revolutionize industries by unlocking the true potential of data.
Breaking Barriers: Fusionex’s Initial Challenges
Overcoming Obstacles
As with any entrepreneurial endeavor, Fusionex faced its fair share of challenges in the early years. Building a successful technology company from scratch is no easy feat, and Teh and his team encountered numerous obstacles along the way. However, their unwavering determination and resilience helped them navigate through the toughest of times, emerging stronger and more determined than ever.
Building Trust
One of the major challenges in the early days was establishing trust in the market. With competition intensifying and skeptical customers wary of unproven solutions, Teh and his team had to work hard to demonstrate the value of Fusionex’s offerings. By consistently delivering reliable and innovative solutions, they gradually won over the trust and confidence of businesses worldwide.

Tech Innovations: Fusionex’s Breakthrough Solutions
Easing Complexity
Fusionex’s journey is characterized by a string of groundbreaking innovations that have redefined the way businesses approach data analytics and digital transformation. Throughout the years, Teh and his team have continuously strived to simplify and democratize complex technologies, making them accessible to businesses of all sizes and industries.
Revolutionizing Industries
From harnessing the power of artificial intelligence and machine learning to developing cutting-edge data management solutions, Fusionex has consistently pushed the boundaries of technological innovation. By enabling businesses to extract actionable insights from vast amounts of data, they have played a pivotal role in transforming industries such as finance, healthcare, and retail.
Expanding Horizons: Fusionex’s Global Reach
A Global Footprint
From its humble beginnings, Fusionex has grown from strength to strength, expanding its presence on a global scale. Today, the company operates in multiple countries, collaborating with businesses across diverse industries to drive digital transformation and achieve sustainable growth.
Embracing Diversity
Fusionex’s global reach is not limited to physical boundaries alone. Teh and his team understand the value of diversity and have fostered a inclusive culture within the organization. By bringing together individuals from different backgrounds, cultures, and perspectives, Fusionex has created a dynamic and innovative workforce that thrives on the power of collaboration.
Leadership Excellence: Ivan Teh’s Strategic Decision-making
Guiding Fusionex’s Path
One of the key factors behind Fusionex’s success is Teh’s exceptional leadership skills and strategic decision-making. Drawing upon his vast knowledge and experience, Teh has guided the company through various stages of growth, ensuring that it remains at the forefront of technological innovation and industry trends.

A People-Centric Approach
Teh believes in the power of people and places great emphasis on building strong relationships with employees, clients, and stakeholders. By fostering a people-centric culture within Fusionex, he has created an environment where individuals can thrive, innovate, and excel. This approach has not only bolstered employee satisfaction but also fueled the company’s growth and success.
Driving Growth: Fusionex’s Expansion Strategy
Strategic Partnerships
To further accelerate its growth and expand its reach, Fusionex has forged strategic partnerships with leading technology companies and industry experts. By combining their expertise, resources, and networks, Fusionex has been able to tap into new markets, explore innovative solutions, and drive mutually beneficial collaborations.
Investing in R&D
Another pillar of Fusionex’s expansion strategy is its unwavering commitment to research and development. Teh and his team understand that technological innovation is a never-ending journey and that continuous investment in R&D is crucial to staying ahead of the curve. By constantly exploring new technologies and enhancing existing solutions, Fusionex remains a frontrunner in the tech industry.
Building a Strong Team: Fusionex’s Company Culture
Nurturing Talent
At the heart of Fusionex’s success lies its strong and talented workforce. Teh firmly believes in nurturing talent and provides numerous opportunities for personal and professional growth. Through mentorship programs, training initiatives, and talent development strategies, Fusionex ensures that its employees are equipped with the skills and expertise needed to drive innovation and deliver exceptional results.
Cultivating Collaboration
Collaboration is deeply ingrained in Fusionex’s company culture. Teh recognizes that true innovation happens when individuals from diverse backgrounds come together, share ideas, and work towards common goals. By fostering a collaborative environment, Fusionex encourages its employees to think outside the box, challenge conventions, and drive collective growth.
Thought Leadership: Ivan Teh’s Contributions to the Tech Industry
Sharing Knowledge
Apart from leading Fusionex to new heights, Teh is also committed to sharing his knowledge and expertise with the wider tech community. Through speaking engagements, publications, and thought leadership initiatives, he strives to inspire and educate aspiring entrepreneurs and industry professionals. By sharing his experiences and insights, Teh hopes to empower others to pursue their entrepreneurial dreams and make a positive impact on the world.
Future Outlook: Fusionex’s Exciting Ventures
Embracing the Future
Looking ahead, Fusionex shows no signs of slowing down. With Teh at the helm, the company continues to explore new frontiers and embrace emerging technologies. From the adoption of blockchain and Internet of Things (IoT) to the integration of virtual reality, Fusionex remains at the cutting edge of innovation, poised to shape the future of technology and drive transformative change across industries.
Building on Success
As Fusionex ventures into new territories and expands its range of products and services, one thing remains constant – its unwavering commitment to excellence and customer satisfaction. Teh and his team understand that success is not a one-time achievement but a continuous pursuit. With a solid foundation, a talented workforce, and a culture of innovation, Fusionex is well-positioned to build on its success and create a future where technology shapes a better world for all.


Understanding Conversational AI: The Future of Chatbots
Have you ever wondered about the future of chatbots and how they are changing the way we interact with technology? In this article, we will explore the world of Conversational AI, a revolutionary technology that is transforming the chatbot industry. From understanding the basics of Conversational AI to its potential applications and benefits, we will provide you with all the information you need to stay ahead in this exciting field. So grab a cup of coffee and get ready to dive into the fascinating world of Conversational AI and discover how it is shaping the future of chatbots.
Understanding Conversational AI: The Future of Chatbots
Artificial Intelligence (AI) has revolutionized the way we interact with technology. One of the exciting advancements in AI is Conversational AI, which focuses on creating chatbots that can engage in human-like conversations. In this article, we will explore the world of Conversational AI, its evolution, advantages, challenges, key technologies, and its applications in various industries. We will also discuss the process of designing, building, and training a Conversational AI model, along with the testing and evaluation aspects. Lastly, we will look into the current trends in Conversational AI and what the future holds for this promising technology.

Introduction to Conversational AI
Conversational AI refers to the development of AI systems that can communicate with humans in a natural and interactive manner. The aim is to create chatbots that can understand human language, respond appropriately, and engage in meaningful conversations. These chatbots can be used for a wide range of applications, from customer service and virtual agents to social media interactions and voice assistants.
Evolution of Chatbots
Chatbots have come a long way since their inception. Initially, they were simple rule-based systems that followed predefined patterns and responded to specific keywords. However, with advancements in AI and Natural Language Processing (NLP), chatbots have evolved to understand and generate human language more effectively. Modern chatbots utilize machine learning techniques and can learn from user interactions to provide more personalized and contextual responses.
Advantages of Conversational AI
Conversational AI offers numerous advantages over traditional methods of human-computer interaction. Firstly, it provides a more natural and intuitive way of interacting with technology, as users can communicate using their own language. This leads to higher user satisfaction and engagement. Secondly, Conversational AI enables businesses to provide 24/7 customer support, without the need for human intervention. This not only reduces costs but also improves the overall customer experience. Additionally, chatbots can handle multiple conversations simultaneously, ensuring faster response times and efficient handling of queries.
Applications of Conversational AI
Conversational AI has found applications in various industries, transforming the way businesses interact with their customers. In the domain of customer service, chatbots can provide instant and accurate responses to frequently asked questions, reducing the load on human agents. Virtual agents, on the other hand, can assist users with tasks such as travel bookings, appointment scheduling, and information retrieval. Social media chatbots are used for engagement and marketing purposes, providing personalized recommendations and addressing customer queries. Lastly, voice assistants like Siri and Alexa have become household names, enabling users to perform tasks such as setting reminders, playing music, and controlling smart devices with voice commands.
Challenges in Developing Conversational AI
While Conversational AI has made significant progress, there are still several challenges in its development. One of the main challenges is achieving accurate and context-aware understanding of user inputs. Natural language is complex, and chatbots must be able to comprehend and interpret various forms of expressions, including slang, sarcasm, and ambiguity. Another challenge is generating meaningful and coherent responses that fit the conversation context. Chatbots should be able to recall previous interactions and maintain a consistent and engaging dialogue. Furthermore, privacy and security concerns must also be addressed, as chatbots handle sensitive user information.
Key Technologies for Conversational AI
Several key technologies form the foundation of Conversational AI. These technologies work together to enable chatbots to understand and respond to human language.
Natural Language Processing (NLP)
NLP is at the core of Conversational AI, as it focuses on the interaction between computers and human language. NLP techniques enable chatbots to understand the meaning behind user inputs and generate appropriate responses. It involves tasks such as tokenization, part-of-speech tagging, named entity recognition, and sentiment analysis.
Speech Recognition
Speech recognition technology allows chatbots to transcribe spoken language into text. It enables voice assistants and systems to understand and interpret voice commands. Advanced speech recognition techniques incorporate machine learning algorithms to improve accuracy and handle various accents and languages.

Machine Learning
Machine learning plays a crucial role in Conversational AI by allowing chatbots to learn from user interactions and improve their performance over time. Supervised learning algorithms can be used to train chatbot models using annotated data, while reinforcement learning techniques enable chatbots to learn through trial and error.
Understanding Human Language
To create more human-like conversations, chatbots must possess an understanding of human language structures, semantics, and pragmatics. This involves knowledge about grammar, syntax, and the ability to handle context-dependent language phenomena.
Designing a Conversational AI System
Designing an effective Conversational AI system requires careful consideration of various factors.
User Interface and Experience
A well-designed user interface is essential for a positive user experience. Chatbots should have a user-friendly interface that allows users to converse seamlessly. The interface should be intuitive and provide clear instructions and suggestions to guide users during conversations.

Personalization and Context
To provide personalized interactions, chatbots should be able to capture and retain user information. They should remember previous interactions and incorporate context to tailor responses accordingly. Personalization enhances user engagement and satisfaction.
Integration with Other Systems
Conversational AI systems often need to integrate with other existing systems and databases to provide accurate and relevant information. Integration with customer relationship management (CRM) systems, ticketing systems, and knowledge bases enables chatbots to access and retrieve data to assist users effectively.
Building and Training a Conversational AI Model
Developing a Conversational AI model involves several stages, from data collection to model deployment and monitoring.
Data Collection and Annotation
To train a chatbot model, a large dataset of conversations is required. This dataset needs to be annotated, with user inputs and corresponding responses labeled for training purposes. Collecting and preparing the right dataset is crucial for building an accurate and context-aware chatbot.

Training Data Preparation
Once the dataset is ready, it needs to be preprocessed and transformed into a suitable format for training. This involves cleaning the data, tokenizing, and encoding the text to create input representations that can be fed into the machine learning model.
Model Building and Validation
Using the prepared training data, a machine learning model is built to learn from the examples and generate responses. The model is trained using supervised or reinforcement learning techniques, and its performance is evaluated through validation and testing. Iterative improvements are made based on the evaluation results.
Deployment and Monitoring of Conversational AI Systems
After the model is trained and validated, it is deployed into a production environment, where it can interact with users in real-time. However, the journey doesn’t end there. Continuous monitoring and maintenance are required to ensure the chatbot performs as expected and to address any issues or improvements.
Testing and Evaluation of Conversational AI Systems
Testing and evaluation are crucial steps to assess the performance and effectiveness of Conversational AI systems. This includes both functional testing, where the system is tested for accuracy and correctness, and user testing, where real users interact with the chatbot to provide feedback and identify areas of improvement.

Current Trends in Conversational AI
Conversational AI is a rapidly evolving field, and several trends are shaping its future.
Voice Assistants
Voice assistants have gained immense popularity, with the introduction of devices like Amazon Echo and Google Home. Voice-powered chatbots are becoming commonplace, allowing users to interact with technology using voice commands. The convenience and hands-free experience offered by voice assistants make them a preferred choice for many users.
Virtual Agents
Virtual agents are being used in various industries, including healthcare, finance, and e-commerce. They assist users with tasks ranging from appointment scheduling to providing product recommendations. Virtual agents combine the advantages of automation and personalization, offering users a seamless and efficient experience.
Customer Service Chatbots
Customer service chatbots have become an integral part of many businesses, providing instant support and assistance. These chatbots handle the initial customer queries, freeing up human agents to handle more complex issues. They can help reduce response times and improve customer satisfaction.
Social Media Chatbots
Social media chatbots have gained popularity as a means of engaging with customers. They can provide personalized recommendations, answer customer queries, and even facilitate transactions. Social media platforms like Facebook Messenger and WhatsApp have integrated chatbots to enhance user experiences.
The Future of Conversational AI
Conversational AI holds great promise, and the future looks incredibly exciting. Here are some areas that will witness significant advancements:
Improved Natural Language Understanding
As NLP techniques continue to advance, chatbots will become even better at understanding and analyzing human language. They will be able to handle nuances, context, and emotions, leading to more efficient and satisfying conversations.
More Human-Like Conversations
The goal of Conversational AI is to make chatbots indistinguishable from human agents. By incorporating more sophisticated dialogue management and natural language generation techniques, chatbots will be able to engage in more realistic and human-like conversations.
Integration with Smart Devices
Conversational AI will play a crucial role in the growing ecosystem of smart devices. Chatbots will seamlessly integrate with various devices, such as smartphones, smartwatches, and home automation systems. This integration will enable users to control their devices through natural language commands.
Mass Adoption of Conversational AI
With advancements in technology and increased user acceptance, Conversational AI is expected to become a mainstream interaction paradigm. Chatbots will be integrated into various industries and applications, ranging from healthcare and education to entertainment and personal assistants.
Conclusion
Conversational AI has transformed the way we interact with technology, enabling chatbots to engage in meaningful conversations with users. The future of Conversational AI looks bright, with advancements in NLP, machine learning, and integration with smart devices. Businesses across industries are adopting this technology to improve customer service, enhance user experiences, and increase efficiency. As the field continues to evolve, Conversational AI will undoubtedly become an integral part of our everyday lives. So embrace this exciting technology and get ready to experience a new era of human-computer interaction.


Demystifying Natural Language Processing: A Comprehensive Guide for Beginners
If you’ve ever wondered about the fascinating world of Natural Language Processing (NLP), look no further. In “Demystifying Natural Language Processing: A Comprehensive Guide for Beginners,” we aim to break down this complex subject into easily digestible pieces. From its definition to its applications, we’ll guide you through the basics of NLP in a friendly and approachable manner. Whether you’re just starting out or already have some knowledge in the field, this comprehensive guide will provide valuable insights and practical tips that will leave you craving for more. So, let’s embark on this journey together and uncover the wonders of Natural Language Processing.
What is Natural Language Processing?
Definition of Natural Language Processing
Natural Language Processing (NLP) is a field of study that focuses on the interaction between computers and human language. It involves the development of algorithms and models to enable computers to understand, interpret, and generate human language in a way that is useful and meaningful.
Importance of Natural Language Processing
Natural Language Processing plays a crucial role in bridging the gap between human communication and computer understanding. Advancements in NLP have revolutionized various industries by enabling machines to process human language for information extraction, sentiment analysis, speech recognition, and many other applications. By leveraging NLP techniques, businesses can gain valuable insights from vast amounts of text data, automate customer service through chatbots, and enhance language-based human-computer interactions.
Applications of Natural Language Processing
NLP has a wide range of applications across various domains. It is used in information retrieval systems to analyze and index text documents. Sentiment analysis and opinion mining, powered by NLP, help companies understand customer feedback and monitor social media sentiment. Machine translation enables automated translation between different languages. NLP techniques are also employed in question-answering systems, chatbots, speech recognition, and text summarization. The applications of NLP continue to expand as technology advances.
History of Natural Language Processing
Origins of Natural Language Processing
The origins of Natural Language Processing can be traced back to the 1950s when computer scientists began exploring ways to enable machines to understand and process language. The early focus was on developing language translation systems, but as the field progressed, researchers realized the complexity and challenges involved in accurately capturing the nuances of human language.
Milestone Developments in Natural Language Processing
Over the years, significant milestones have marked the progress of Natural Language Processing. In 1950, Alan Turing proposed the “Turing Test” as a measure of machine intelligence in language understanding. In the 1960s and 1970s, early attempts at machine translation and language understanding systems were made. The 1980s brought advances in syntax-based parsing algorithms. The 1990s witnessed the emergence of statistical approaches to language processing, with research focusing on machine learning techniques.
Advancements in Natural Language Processing
With the proliferation of vast amounts of digital data and the advancements in computing power, Natural Language Processing has witnessed tremendous progress in recent years. Deep learning models, such as recurrent neural networks (RNNs) and transformer models, have significantly improved language understanding capabilities. NLP techniques have become more accessible, with the development of open-source libraries and frameworks, empowering developers to incorporate language processing functionalities into their applications.

Understanding the Basics of Natural Language Processing
Components of Natural Language Processing
Natural Language Processing consists of several key components that enable computers to process and understand human language. These components include tokenization, part-of-speech tagging, syntax analysis, semantic analysis, and discourse understanding. Each component plays a vital role in the overall language processing pipeline, contributing to the extraction of meaning and context from textual data.
Tokenization and Text Preprocessing
Tokenization is the process of dividing text into smaller units, known as tokens. These tokens can be individual words, phrases, or even sentences. Tokenization is a crucial initial step in NLP, as it breaks down the text into manageable and meaningful units for further analysis. Text preprocessing involves tasks like removing punctuation, converting text to lowercase, and eliminating stop words to enhance the accuracy of downstream language processing tasks.
Part-of-Speech Tagging and Morphology
Part-of-speech tagging assigns grammatical labels, such as noun, verb, adjective, etc., to each word in a sentence. It helps in understanding the syntactic structure of a sentence and is useful in tasks like text-to-speech synthesis, information retrieval, and grammar checking. Morphology, another important component, deals with the internal structure and formation of words. It involves tasks like stemming (reducing words to their base or root form) and lemmatization (replacing words with their dictionary form).
Syntax and Parsing
Syntax analysis involves understanding the grammatical structure of a sentence and the relationships between its constituent words. Parsing algorithms, such as the constituency and dependency parsers, analyze the syntactic structure of sentences. Syntax analysis is critical for tasks like machine translation, information extraction, and text summarization.
Semantic and Pragmatic Analysis
Semantic analysis aims to understand the meaning of words and sentences in a particular context. It involves tasks like named entity recognition (identifying and classifying named entities like person names, organization names, etc.), word sense disambiguation (determining the correct meaning of a word based on context), and semantic role labeling (assigning roles to words in a sentence). Pragmatic analysis focuses on understanding the intended meaning and context beyond the literal interpretation of language.
Discourse Understanding
Discourse understanding involves analyzing the structure and coherence of larger pieces of text, such as paragraphs, articles, or conversations. It aims to understand how different sentences or utterances relate to each other within a broader context. Discourse understanding is important for applications like summarization, dialogue systems, and question-answering.
Machine Learning and Natural Language Processing
Machine Learning Techniques in Natural Language Processing
Machine learning plays a significant role in Natural Language Processing, enabling computers to learn from data and make accurate predictions or classifications. Supervised learning, unsupervised learning, semi-supervised learning, and deep learning are commonly used techniques in NLP.
Supervised Learning
Supervised learning involves training a model on labeled data, where each data point is associated with a specific label or class. In NLP, supervised learning is used for tasks like sentiment analysis, text classification, named entity recognition, and part-of-speech tagging. The model learns patterns and relationships in the labeled data, allowing it to make predictions on new, unseen data.
Unsupervised Learning
Unsupervised learning involves training a model on unlabeled data, where the model learns patterns and structures in the data without predefined labels. Unsupervised learning is commonly used for tasks like clustering similar documents, topic modeling, and word embeddings. It helps in discovering hidden patterns and structures in textual data, leading to a better understanding of the data.
Semi-Supervised Learning
Semi-supervised learning is a combination of supervised and unsupervised learning. It leverages a small amount of labeled data along with a larger amount of unlabeled data for training. Semi-supervised learning is useful when obtaining a large amount of labeled data is expensive or time-consuming. It allows the model to benefit from both labeled and unlabeled data, improving performance and efficiency.
Deep Learning in Natural Language Processing
Deep learning, a subset of machine learning, involves training deep neural networks with multiple hidden layers to learn complex patterns and representations. Deep learning models, such as recurrent neural networks (RNNs) and transformer models (e.g., BERT, GPT), have revolutionized Natural Language Processing. These models have shown exceptional performance in tasks like machine translation, sentiment analysis, and natural language understanding.

Common Challenges in Natural Language Processing
Ambiguity in Language
One of the fundamental challenges in Natural Language Processing is the ambiguity of language. Words and phrases can have multiple meanings depending on the context. Resolving this ambiguity requires advanced algorithms and techniques, such as word sense disambiguation, contextual embeddings, and domain-specific knowledge.
Word Sense Disambiguation
Word sense disambiguation is the task of determining the correct meaning of a word based on its context within a sentence. It is crucial for accurate language understanding and plays a significant role in tasks like machine translation, sentiment analysis, and information retrieval. Various algorithms and approaches, including supervised and unsupervised methods, have been developed for word sense disambiguation.
Dealing with Noise and Outliers
Text data often contains noise, outliers, and inconsistencies, which can affect the performance of Natural Language Processing models. Noise can include misspelled words, grammatical errors, colloquial expressions, and slang. Robust preprocessing techniques, such as spell checking, error correction, and data cleaning, are essential for handling noise and ensuring accurate language processing.
Handling Large Volumes of Data
The exponential growth of digital data presents a challenge in terms of processing and analyzing large volumes of text data. Natural Language Processing techniques need to be scalable and efficient to handle big data. Distributed computing frameworks, parallel processing, and optimization techniques are utilized to handle the computational demands of processing massive amounts of text data.
Multilingual Natural Language Processing
Natural Language Processing becomes more complex when dealing with multiple languages. Each language has its own grammar, syntax, and nuances. Multilingual NLP involves developing models and algorithms that can handle multiple languages, enabling tasks like machine translation, sentiment analysis, and information retrieval across diverse language datasets.
Tools and Libraries for Natural Language Processing
Popular Programming Languages for Natural Language Processing
Several programming languages are commonly used for Natural Language Processing. Python, with its rich ecosystem of libraries and frameworks, including NLTK (Natural Language Toolkit) and spaCy, is widely favored by NLP practitioners. Java is also popular in NLP, supported by libraries like Apache OpenNLP and Stanford NLP. R, with its statistical capabilities, is often used for text classification and sentiment analysis.
Python-based Libraries and Frameworks
Python offers a variety of powerful libraries and frameworks for Natural Language Processing. NLTK, a comprehensive library, provides tools and resources for tasks like tokenization, text preprocessing, part-of-speech tagging, and named entity recognition. spaCy is another popular library that offers efficient syntax and semantic analysis capabilities. Transformers, built on the PyTorch framework, provides state-of-the-art models for tasks like machine translation and language generation.
Java-based Libraries and Frameworks
Java-based libraries and frameworks are widely used in NLP research and development. Apache OpenNLP is a popular choice, offering various natural language processing tools and models. Stanford NLP provides a suite of Java libraries for tasks like tokenization, part-of-speech tagging, and named entity recognition. These libraries have extensive documentation and community support, making them valuable resources for NLP practitioners.
R Tools and Packages
R, a statistical programming language, has a growing number of tools and packages for Natural Language Processing. The tm package provides functions for text mining tasks like document cleaning, tokenization, and term frequency analysis. The tidytext package, built on the principles of the tidyverse, offers a tidy data approach to text analysis and manipulation. RTextTools and caret are other notable packages for text classification and sentiment analysis.
Natural Language Processing APIs
In addition to libraries and frameworks, several Natural Language Processing APIs are available, offering pre-trained models and simplified interfaces for performing language processing tasks. Microsoft Azure Text Analytics API, Google Cloud Natural Language API, and IBM Watson Natural Language Understanding API are popular choices for accessing NLP functionalities in a cloud-based environment. These APIs provide convenient and scalable solutions for integrating NLP capabilities into applications and services.
Ethical Considerations in Natural Language Processing
Bias and Fairness in Natural Language Processing
Bias and fairness are important ethical considerations in Natural Language Processing. Language models can inadvertently replicate and reinforce societal biases present in the data they are trained on. It is crucial to address and mitigate bias in language processing algorithms to ensure fairness and prevent discriminatory outcomes. Ethical guidelines and principles, along with diverse training data, can help in reducing bias.
Privacy and Data Protection
Natural Language Processing involves the processing of text data, which may contain sensitive information. Privacy and data protection need to be prioritized to ensure the responsible handling of personal and confidential data. Appropriate security measures, data anonymization techniques, and compliance with privacy regulations are essential in NLP systems that handle user-generated data.
Transparency and Accountability
Transparency and accountability are crucial in Natural Language Processing systems. Users should have visibility into how their data is being processed and used. Developers and organizations should be transparent about the algorithms and models used in their NLP systems, as well as the limitations and potential biases associated with them. Accountability and clear communication are essential for building trust with users.
Addressing Social and Cultural Biases
Natural Language Processing models can inadvertently perpetuate social and cultural biases present in the training data. It is important to address these biases and ensure inclusivity and fairness in language processing systems. Diversity in the training data, bias detection algorithms, and ongoing evaluation and improvement of models are necessary steps to mitigate social and cultural biases.
Future Trends in Natural Language Processing
Conversational AI and Chatbots
Conversational AI, powered by Natural Language Processing, is a rapidly evolving field. Chatbots, virtual assistants, and voice-based interfaces are becoming increasingly intelligent and human-like in their interactions. Future advancements in Natural Language Processing will focus on enhancing the conversational capabilities of AI systems, enabling more natural and context-aware conversations.
Advances in Voice Recognition and Natural Language Understanding
Voice recognition technology has already made significant strides, with systems like Siri, Google Assistant, and Amazon Alexa becoming common in everyday life. The future of Natural Language Processing will involve refining voice recognition algorithms, improving accuracy, and adapting to different accents and languages. Natural language understanding algorithms will also evolve to better interpret and respond to spoken language.
Deep Learning Models and Transformers
Deep learning models, such as transformer models, have had a profound impact on Natural Language Processing. The success of models like BERT and GPT has paved the way for further advancements in language understanding and generation. Future trends will involve the development of more efficient and powerful transformer models that can handle complex language tasks with increased speed and accuracy.
Integration of NLP with Other AI Technologies
Natural Language Processing is increasingly being integrated with other AI technologies, such as computer vision and robotics, to create more comprehensive and intelligent systems. By combining language understanding with image and sensor data, NLP can enable machines to extract information from multimodal inputs, leading to enhanced perception and decision-making capabilities.

Real-World Applications of Natural Language Processing
Sentiment Analysis and Opinion Mining
Sentiment analysis and opinion mining involve the extraction of subjective information from text data, enabling businesses to understand customer sentiment and opinions. NLP techniques are used to analyze social media posts, customer reviews, and feedback to gain insights into customer satisfaction, brand perception, and market trends. This information is valuable for making informed business decisions and improving customer experiences.
Text Classification and Topic Modeling
Text classification involves categorizing text documents into predefined classes or categories. NLP algorithms are used for tasks like news categorization, spam detection, sentiment classification, and customer support ticket routing. Topic modeling, on the other hand, aims to discover underlying themes or topics within a collection of documents, helping in tasks like document clustering, content recommendation, and trend analysis.
Question-Answering Systems
Question-answering systems leverage NLP techniques to automatically extract relevant information from textual data and generate meaningful responses to user queries. These systems can be implemented in various domains, such as customer support, virtual assistants, and information retrieval. Advanced question-answering systems utilize machine learning and deep learning models to improve accuracy and understand complex queries.
Machine Translation
Machine translation is the task of automatically translating text from one language to another. NLP techniques, including statistical and neural machine translation models, are used to build language translation systems. These systems have practical applications in areas like international communication, cross-language information retrieval, and localization of software and content.
Speech Recognition and Synthesis
Speech recognition and synthesis involve converting spoken language into written text and vice versa. Natural Language Processing techniques are used to develop accurate and efficient speech recognition systems, which find applications in voice assistants, transcription services, and voice-controlled interfaces. Speech synthesis, also known as text-to-speech, utilizes NLP models to convert written text into spoken words, enabling applications like speech-enabled navigation systems and audiobook production.
Conclusion
Summary of Natural Language Processing
Natural Language Processing is a field that focuses on enabling computers to understand and process human language. It plays a crucial role in various applications, ranging from sentiment analysis and information retrieval to machine translation and chatbots. NLP involves components such as tokenization, part-of-speech tagging, syntax analysis, semantic analysis, and discourse understanding, all of which contribute to the extraction of meaning and context from textual data. Machine learning techniques, including supervised learning, unsupervised learning, semi-supervised learning, and deep learning, are used to enhance language processing capabilities.
Implications and Impact of Natural Language Processing
Natural Language Processing has revolutionized the way humans interact with computers and has opened up new opportunities for businesses and researchers. It enables organizations to derive insights from text data, automate customer service, and improve language-based human-computer interactions. NLP also brings challenges like dealing with ambiguity in language, addressing bias and fairness, and handling large volumes of data. Ethical considerations, such as privacy, transparency, and cultural biases, also need to be taken into account.
Future Opportunities and Challenges
The future of Natural Language Processing holds exciting possibilities. Chatbots and conversational AI will become more advanced and human-like, while voice recognition and natural language understanding will continue to improve. Deep learning models and transformers will push the boundaries of language understanding, and integration with other AI technologies will pave the way for comprehensive intelligent systems. However, challenges like ensuring fairness, reducing biases, and handling multilingual processing will remain areas of focus. Natural Language Processing will continue to evolve, shaping the future of human-computer interaction.
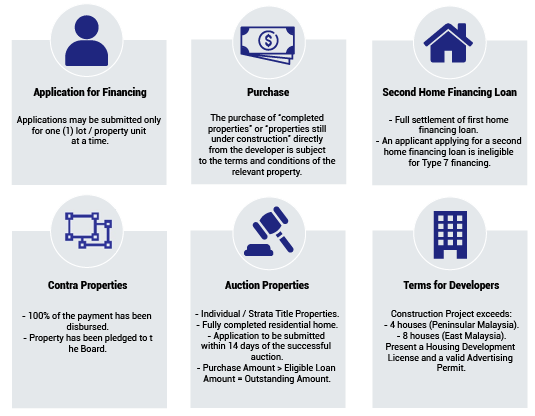

A Comprehensive Guide to Home Financing Options in Malaysia
Looking to buy a home in Malaysia but feeling overwhelmed by the plethora of financing options available? Don’t worry, we’ve got you covered! In this comprehensive guide, we’ll walk you through the various home financing options in Malaysia, providing you with all the information you need to make an informed decision. From H1 tags to H3 tags, each article is carefully structured to ensure easy navigation and understanding. With a minimum of 2500 words per article, we delve into the world of home financing in a friendly and approachable tone, making it a breeze for you to explore further. So grab a cup of tea, sit back, and let’s dive into the exciting world of home financing options in Malaysia!
A Comprehensive Guide to Home Financing Options in Malaysia
Buying a home is an exciting milestone in your life, but it can also be a complex and overwhelming process. One of the most crucial aspects of purchasing a property is securing the right home financing option. With so many choices available in Malaysia, it’s essential to have a clear understanding of the various home financing options before making your decision. In this comprehensive guide, we will explore the different types of home loans and financing schemes available to help you make an informed choice.
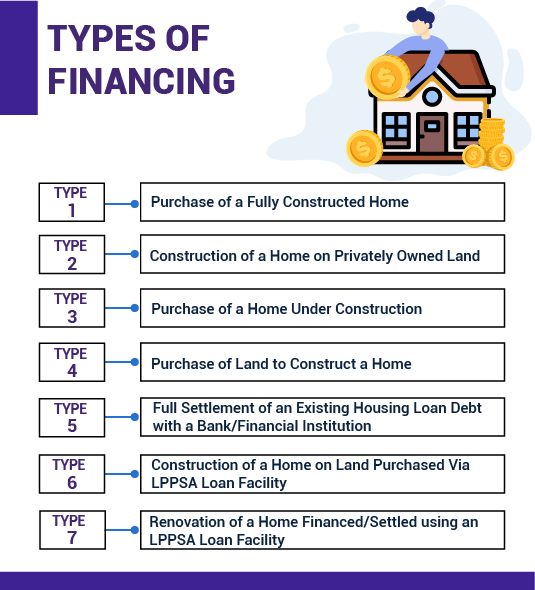
1. Conventional Home Loans
1.1 Overview of Conventional Home Loans
Conventional home loans are the most common type of financing option in Malaysia. They are offered by banks and financial institutions and are governed by the standard lending practices. Conventional home loans are not linked to any specific religious or cultural requirements and are suitable for individuals of all backgrounds.
1.2 Features and Benefits
Conventional home loans come with several features and benefits that make them a popular choice among homebuyers. These include flexible repayment options, competitive interest rates, and the ability to prepay the loan without incurring any penalties. Additionally, conventional home loans can be used to finance all types of residential properties, such as landed houses, apartments, and condominiums.
1.3 Eligibility Criteria
To be eligible for a conventional home loan, you generally need to meet certain criteria set by the lending institution. This includes having a stable source of income, a satisfactory credit history, and a reasonable debt-to-income ratio. The specific eligibility criteria may vary between lenders, so it’s important to check with the chosen institution to ensure you meet their requirements.
1.4 Application Process
When applying for a conventional home loan, you will typically need to provide the lender with various documents, such as proof of identity, income statements, and property details. The application process may involve a thorough assessment of your financial situation, creditworthiness, and the property you intend to purchase. It’s essential to gather all the necessary documents and submit them accurately to expedite the loan approval process.
1.5 Pros and Cons
Like any other financing option, conventional home loans have their advantages and disadvantages. Some of the pros include the flexibility to choose from a wide range of lenders, competitive interest rates, and the potential for higher loan amounts. However, one of the downsides of conventional home loans is that they do not cater to individuals with specific religious requirements. Additionally, the approval process may involve strict eligibility criteria and a longer time frame compared to other financing options.
2. Islamic Home Financing
2.1 Introduction to Islamic Home Financing
Islamic home financing, also known as Shariah-compliant financing, is a type of home loan that adheres to the principles of Islamic finance. It caters to individuals who prefer financing options that align with their religious beliefs. Islamic home financing operates on the concept of profit and risk-sharing, rather than interest-based lending.
2.2 Principles of Islamic Financing
Islamic home financing is guided by principles outlined in Islamic law, known as Shariah. The key principles include the prohibition of charging or receiving interest (riba), the avoidance of uncertainty (gharar), and the prohibition of investment in unethical activities (haram). Instead, Islamic home financing utilizes concepts such as profit-sharing (mudarabah), cost-plus financing (murabahah), and leasing (ijara) to facilitate the purchase of a property.
2.3 Types of Islamic Home Financing
There are different types of Islamic home financing options available in Malaysia, each with its own unique features. Some popular options include Musharakah Mutanaqisah, Ijarah Muntahiyah Bittamlik, and Bay’ Bithaman Ajil. These options offer variations in terms of profit-sharing, ownership structure, and payment methods, allowing borrowers to choose an option that best suits their needs.
2.4 Eligibility and Documentation
The eligibility criteria and documentation requirements for Islamic home financing are similar to conventional home loans. Borrowers need to have a stable income, good credit history, and meet the lender’s specific requirements. In addition, Islamic home financing may require additional documentation related to the specific Islamic finance principles being applied.
2.5 Comparison with Conventional Home Loans
Islamic home financing differs from conventional home loans primarily in the way the loans are structured and the principles they abide by. While conventional home loans charge interest, Islamic home financing uses alternative methods such as profit-sharing or cost-plus financing. Additionally, Islamic home financing caters to individuals with specific religious requirements, providing an alternative for those who want to ensure adherence to Islamic principles.
3. Fixed-Rate Home Loans
3.1 Basics of Fixed-Rate Home Loans
Fixed-rate home loans are a popular choice for individuals seeking stability and predictability in their loan repayments. With a fixed-rate loan, the interest rate remains constant throughout the loan tenure, allowing borrowers to plan their finances with confidence. This is in contrast to variable-rate loans, where the interest rate can fluctuate over time.
3.2 Advantages and Disadvantages
One of the advantages of a fixed-rate home loan is that it provides borrowers with a consistent repayment amount, making it easier to budget and manage finances. It also offers protection against potential interest rate hikes, as borrowers are not affected by market fluctuations. However, the downside of fixed-rate home loans is that they typically come with higher interest rates compared to variable-rate loans. Additionally, borrowers may miss out on potential savings if interest rates decrease during the loan tenure.
3.3 Choosing the Right Terms and Tenure
When opting for a fixed-rate home loan, it’s crucial to carefully consider the loan terms and tenure. The loan term refers to the duration over which the loan will be repaid, while the loan tenure determines the number of years it will take to fully repay the loan. It’s important to strike a balance between a shorter loan term, which may result in higher monthly repayments, and a longer loan term, which may result in higher overall interest payments.
3.4 Application Process
The application process for a fixed-rate home loan is similar to other home loans. Borrowers need to provide the necessary documentation, such as proof of identity, income statements, and property details. Lenders will assess the borrower’s eligibility based on factors such as creditworthiness, debt-to-income ratio, and employment stability. Once approved, the loan agreement will outline the fixed interest rate, loan terms, and repayment schedule.
3.5 Understanding the Loan Repayment
With a fixed-rate home loan, the repayment amount remains consistent throughout the loan tenure. Borrowers make regular monthly payments that include both the principal amount and the fixed interest rate. By understanding the loan repayment structure, borrowers can effectively plan their finances and ensure timely repayment to avoid any penalties or defaults.
4. Variable-Rate Home Loans
4.1 Introduction to Variable-Rate Home Loans
Variable-rate home loans, also known as adjustable-rate mortgages, are loans with interest rates that can change over time. Unlike fixed-rate loans, where the interest rate is locked in for the entire loan tenure, variable-rate loans are subject to market fluctuations and adjustments based on economic factors.
4.2 How the Interest Rates are Determined
The interest rates for variable-rate home loans are typically tied to a benchmark rate, such as the Base Rate (BR) or the Islamic Financing Rate (IFR), set by the respective financial institution. The benchmark rate is influenced by factors such as economic conditions, inflation, and monetary policy. When the benchmark rate changes, the interest rate on the variable-rate home loan will adjust accordingly.
4.3 Pros and Cons
Variable-rate home loans offer several advantages. Initially, the interest rates are typically lower compared to fixed-rate loans, allowing borrowers to enjoy lower monthly repayments. Additionally, if interest rates decrease over time, borrowers may benefit from reduced repayment amounts. However, one of the drawbacks of variable-rate loans is the uncertainty associated with fluctuating interest rates. Borrowers need to be prepared for the possibility of higher repayment amounts if interest rates rise.
4.4 Factors to Consider Before Opting for Variable Rates
Before considering a variable-rate home loan, it’s important to assess your risk tolerance and financial capability to handle potential interest rate fluctuations. Borrowers should analyze market conditions, economic forecasts, and consult with financial advisors to make an informed decision. Understanding the potential impact of interest rate changes on your monthly budget and overall financing can help mitigate any future financial strain.
4.5 Risks and Rewards
Variable-rate home loans carry inherent risks and rewards. The reward lies in the potential for lower initial interest rates and the possibility of saving money if interest rates decrease. However, there is also the risk of higher interest rates, leading to increased monthly repayments. Borrowers need to carefully weigh the risks and rewards, considering their financial goals and the long-term impact of possible interest rate fluctuations on their overall repayment strategy.

5. Flexi Home Loans
5.1 Understanding Flexi Home Loans
Flexi home loans, also known as flexible home loans, offer borrowers greater control and flexibility over their loan repayments. These loans are designed to provide more options and features that cater to individual financial needs and circumstances.
5.2 Benefits and Features
Flexi home loans offer various benefits and features that make them an attractive option for borrowers. Some of these benefits include the option to make extra repayments, withdraw excess payments, and the potential to reduce the overall interest paid. Flexi home loans also allow borrowers to make changes to their repayment schedules, such as adjusting the loan tenure or taking repayment breaks during emergencies.
5.3 How It Works
Flexi home loans operate on the concept of an overdraft facility linked to the borrower’s home loan account. Any excess funds deposited into the account can be used to offset the outstanding loan amount, effectively reducing the loan tenure and overall interest paid. Borrowers can also withdraw the excess funds if needed, providing a safety net during financial emergencies.
5.4 Eligibility and Considerations
The eligibility criteria for flexi home loans are similar to other home loan options. Borrowers need to meet the lender’s requirements in terms of income, credit history, and property details. It is important to consider factors such as the annual fee, late payment charges, and minimum balance requirements associated with the flexi home loan facility. It’s also essential to evaluate your financial capability to take advantage of the flexibility offered by this loan option effectively.
5.5 Repayment Options and Strategies
With flexi home loans, borrowers have the flexibility to choose from different repayment options and strategies. They can opt for regular monthly repayments or make extra repayments whenever they have surplus funds. The extra repayments can help offset the loan principal and reduce the overall interest paid. Borrowers can also take advantage of features like the redeposit facility, which allows any withdrawn excess funds to be redeposited into the loan account, further reducing the interest payable.
6. Government Home Financing Schemes
6.1 My First Home Scheme
The My First Home Scheme is a government initiative aimed at assisting first-time homebuyers in Malaysia. It is designed to make homeownership more accessible to young individuals or families who have yet to own a property. The scheme offers various benefits such as financing up to 100% of the property value, preferential interest rates, and longer loan tenures.
6.2 PR1MA Home Financing
PR1MA Home Financing is a government initiative managed by PR1MA, the 1Malaysia People’s Housing Programme. The program provides affordable housing options for middle-income individuals and families in Malaysia. PR1MA Home Financing offers attractive financing packages, including high loan-to-value ratios, competitive interest rates, and flexible repayment options.
6.3 First Home Deposit Funding Scheme (MyDeposit)
The First Home Deposit Funding Scheme, also known as MyDeposit, is an initiative aimed at assisting first-time homebuyers in saving for the deposit required to purchase a property. Under the scheme, eligible individuals can receive financial assistance in the form of a 10% deposit, up to a maximum of RM30,000. MyDeposit helps bridge the affordability gap and makes homeownership more attainable for aspiring homeowners.
6.4 Skim Rumah Pertamaku
Skim Rumah Pertamaku, or My First Home Scheme (SRP), is another initiative introduced by the government to assist first-time homebuyers. The scheme offers various incentives and benefits, including higher loan limits, lower interest rates, and partial stamp duty exemptions. The SRP aims to encourage homeownership among first-time buyers and provide them with the necessary financial support to enter the property market.
6.5 Other Government Initiatives
In addition to the aforementioned schemes, there are other government initiatives aimed at promoting homeownership and providing affordable housing options. These include programs such as Rumah Selangorku, Program Perumahan Rakyat, and various state-sponsored affordable housing schemes. Each program has its own eligibility criteria, benefits, and guidelines, catering to different segments of the population based on income levels and geographical locations.
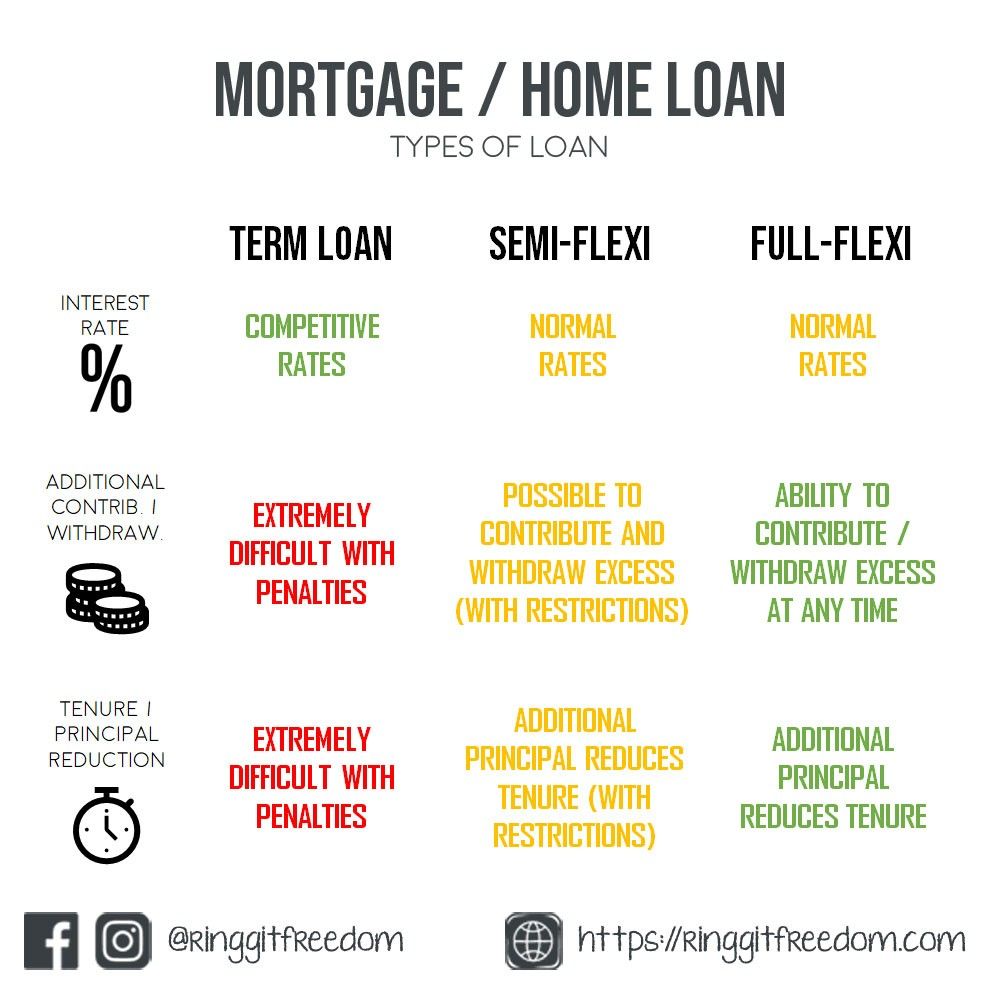
7. Home Loan Refinancing
7.1 Reasons for Refinancing
Home loan refinancing refers to the process of replacing an existing home loan with a new loan from another lender. There are several reasons why borrowers choose to refinance their home loans. These include obtaining a better interest rate, reducing monthly repayments, consolidating debts, accessing additional funds for home improvements, or changing loan tenure to better suit their financial goals.
7.2 When to Refinance
Deciding when to refinance your home loan depends on various factors, such as prevailing interest rates, your financial situation, and the costs associated with refinancing. It’s essential to assess whether refinancing will result in significant savings or benefits that outweigh the costs involved. Refinancing at the right time can potentially help you secure better loan terms and optimize your overall financial position.
7.3 Benefits and Drawbacks
Refinancing a home loan can offer several benefits, including the potential for lower interest rates, reduced monthly repayments, and access to additional funds. It can also help consolidate debts and improve your overall financial management. However, there are also drawbacks to consider, such as upfront costs, potential penalties for early loan repayment, and the impact on your credit score. It’s important to weigh these factors before deciding to refinance.
7.4 The Refinancing Process
The refinancing process involves several steps, including researching and comparing different lenders, gathering the necessary documentation, submitting an application, and undergoing a credit assessment. If approved, the new lender will pay off your existing loan, and you will start making repayments to the new lender under the new loan terms. It’s essential to carefully review the new loan agreement and understand the terms and conditions before finalizing the refinancing process.
7.5 Tips for Successful Refinancing
To ensure a successful refinancing experience, it’s important to follow a few tips. Start by conducting thorough research and comparing various lenders to find the most favorable terms and conditions. Prepare all the necessary documents in advance to streamline the application process. Assess your financial situation and goals to determine if refinancing aligns with your needs. Finally, consult with a financial advisor to fully understand the implications of refinancing and make an informed decision.
8. Home Equity Financing
8.1 Understanding Home Equity
Home equity refers to the portion of your property value that you own outright. It is the difference between the market value of your property and the outstanding amount of your home loan. Home equity increases as you make mortgage repayments and with any appreciation in property value.
8.2 Home Equity Loan vs. Home Equity Line of Credit
Home equity financing, also known as a home equity loan or a home equity line of credit (HELOC), allows homeowners to borrow against the equity in their property. A home equity loan provides a lump sum amount with fixed repayments, while a HELOC offers a revolving line of credit that can be drawn from as needed. Homeowners can choose the option that best suits their financial needs and goals.
8.3 Uses of Home Equity Financing
Home equity financing can be used for various purposes, including home improvements, debt consolidation, education expenses, or emergency funds. The funds obtained through home equity financing can provide homeowners with the flexibility and convenience to access cash when needed, often at lower interest rates compared to other forms of borrowing.
8.4 Eligibility and Application Process
To be eligible for home equity financing, homeowners typically need to have a minimum level of equity built up in their property. Lenders may have specific requirements regarding loan-to-value ratios and creditworthiness. The application process involves submitting the necessary documentation, undergoing a credit assessment, and having the property independently valued to determine the available equity.
8.5 Considerations and Risks
Home equity financing carries certain considerations and risks. Borrowing against your home equity means using your property as collateral, putting it at risk in case of default. It’s crucial to carefully consider the purpose and necessity of borrowing against your home equity and ensure that the repayment terms are manageable within your financial means. Additionally, fluctuations in property value can impact the available equity and borrowing capacity.
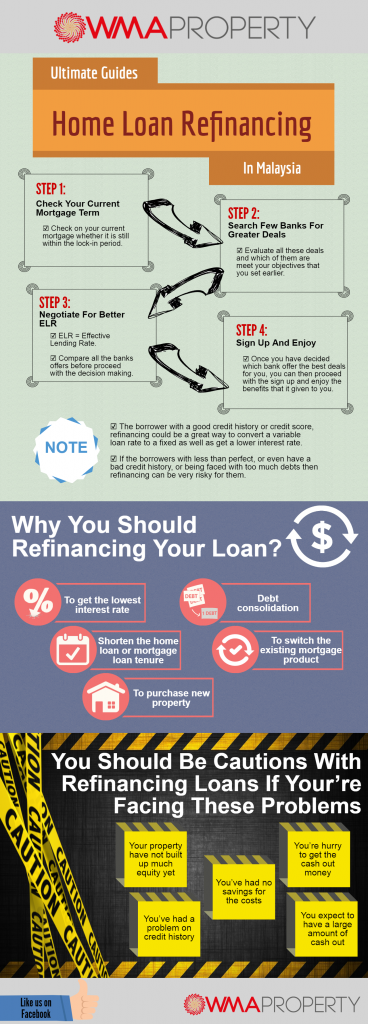
9. Bridging Loans
9.1 Overview of Bridging Loans
Bridging loans are short-term financing options designed to help borrowers bridge the financial gap between the purchase of a new property and the sale of their existing property. These loans provide temporary funding to cover the down payment or purchase price of the new property until the proceeds from the sale are received.
9.2 When to Use Bridging Loans
Bridging loans are typically used in situations where the timing of property transactions does not align. For example, if you have found your dream home but have not yet sold your current property, a bridging loan can provide the necessary funds to secure the new property while you wait for the sale proceeds.
9.3 How Bridging Loans Work
Bridging loans work by providing borrowers with short-term financing in the form of a loan secured against the property being purchased. The loan is typically repaid when the proceeds from the sale of the existing property are received. Bridging loans can be structured with several repayment options, such as monthly interest payments or deferred repayment until the sale is finalized.
9.4 Eligibility Criteria
Eligibility for bridging loans is generally based on the value of the existing property, the loan-to-value ratio, and the borrower’s ability to repay the loan. Lenders will also consider factors such as the expected sale price and timeline of the existing property sale. It’s important to note that bridging loans typically have higher interest rates and additional fees compared to traditional home loans.
9.5 Repayment and Risks
Repayment of a bridging loan occurs once the proceeds from the sale of the existing property are received. The loan terms will specify the repayment structure, which may include the payment of interest only during the bridging period or the accumulation of interest that is repaid at the end of the loan term. It’s important to carefully consider the risks associated with bridging loans, such as changes in property market conditions or delays in the sale of the existing property.
10. Construction Loans
10.1 Introduction to Construction Loans
Construction loans are specifically designed to finance the construction or renovation of a property. These loans provide funds in stages to cover the costs associated with the different phases of the construction project. Construction loans are temporary in nature and are generally converted to long-term financing, such as a conventional home loan, once the construction is completed.
10.2 Process and Stages of Construction Loans
Construction loans typically involve a phased release of funds based on the construction progress. The loan disbursement is structured in stages, such as land purchase, foundation, roof completion, and final completion. Each stage requires verification and inspection by the lender to ensure that the construction is progressing as planned. The funds are released to the borrower or directly to the contractor based on the completion of each stage.
10.3 Loan Disbursement Methods
The disbursement of funds in construction loans can be managed in different ways. One method involves the lender directly making payments to the contractor or suppliers based on invoices and receipts. Another method, known as the reimbursement method, requires the borrower to make the payments and submit reimbursement requests to the lender for approved amounts. The chosen method will depend on the agreement between the lender, borrower, and contractor.
10.4 Eligibility and Documentation
Eligibility for construction loans is based on factors such as the borrower’s financial capability, creditworthiness, and the feasibility of the construction project. Lenders will typically require a detailed construction plan, cost estimates, and the necessary permits or approvals. Providing accurate and comprehensive documentation is essential to facilitate the loan approval process and ensure smooth disbursement of funds.
10.5 Managing Construction Loan Risks
Construction loans come with inherent risks that borrowers need to be aware of. These risks can include cost overruns, delays in construction, or failure to complete the project. It’s important to work with reputable contractors, obtain all necessary permits, and have contingency plans to address any unforeseen challenges. Regular communication with the lender and proactive management of the construction project can help mitigate risks and ensure a successful outcome.
In conclusion, choosing the right home financing option is a crucial decision that can impact your financial well-being for years to come. It’s important to explore and understand the various options available in Malaysia, considering factors such as your financial situation, long-term goals, and specific requirements. By being well-informed and seeking professional advice when needed, you can navigate the home financing landscape with confidence and make an informed decision that suits your needs and aspirations.


The Top Real Estate Developers Revolutionizing the Malaysian Market
Are you curious about the real estate developers who are reshaping the Malaysian market? Look no further! In this article, we will take a closer look at the top developers who are making waves in the industry. From their innovative projects to their commitment to quality, these developers are revolutionizing the way Malaysians experience and invest in properties. Whether you are an aspiring homeowner or a seasoned investor, join us as we explore the exciting world of Malaysia’s top real estate developers.
The Top Real Estate Developers Revolutionizing the Malaysian Market
When it comes to real estate development in Malaysia, there are several notable players who have made a significant impact on the industry. These developers have not only transformed the skyline but have also shaped the way people live and work in the country. In this article, we will explore the top real estate developers in Malaysia and delve into their history, notable projects, and future plans.

how do I calculate roi for property malaysia
1. Sunway Group
The history and background of Sunway Group
Sunway Group is a conglomerate that has become one of the most prominent real estate developers in Malaysia. Established in 1974, the group started as a small tin mining company and eventually diversified into various industries. Led by its visionary founder, Tan Sri Dr. Jeffrey Cheah, Sunway Group has grown into a multi-billion dollar organization with a strong presence in property development, construction, hospitality, and education.
Notable real estate developments by Sunway Group
Sunway Group is renowned for its impressive portfolio of real estate developments. One of their most notable projects is the Sunway City, an integrated township that has become an iconic landmark in Malaysia. Spanning over 800 acres, Sunway City is a live, work, and play community that features residential units, commercial spaces, malls, hospitals, and educational institutions.
The impact of Sunway Group on the Malaysian market
The Sunway Group’s commitment to sustainability and innovation has had a profound impact on the Malaysian real estate market. They have set new benchmarks for eco-friendly development practices and have received numerous accolades for their efforts in creating sustainable communities. Additionally, their dedication to providing world-class amenities and facilities has elevated the standards of living in Malaysia.
Future projects and plans by Sunway Group
Sunway Group has ambitious plans for the future. They are currently involved in several large-scale projects, including the development of new integrated townships, residential properties, and commercial hubs. The group also has a strong focus on expanding their presence internationally, with plans to bring their unique brand of holistic development to other countries.
2. IOI Properties Group
Introduction to IOI Properties Group
IOI Properties Group is another major player in the Malaysian real estate industry. Established in 1984, the group has built a reputation for delivering high-quality residential, commercial, and industrial properties. With a strong emphasis on sustainability and innovation, IOI Properties Group has become synonymous with creating vibrant, well-planned developments.
Highlights of IOI Properties Group’s real estate projects
IOI Properties Group boasts an impressive portfolio of projects that cater to different segments of the market. One of their notable developments is IOI City Mall, a sprawling shopping complex that has become a popular retail and leisure destination. The group has also undertaken several residential projects, offering a wide range of housing options to suit different lifestyles and budgets.
IOI Properties Group’s contributions to the Malaysian market
IOI Properties Group has made significant contributions to the Malaysian real estate market. Their commitment to sustainable development has resulted in the creation of eco-friendly communities that prioritize green spaces and energy efficiency. Additionally, their developments have contributed to the economic growth of the surrounding areas, attracting businesses, residents, and tourists alike.
Upcoming developments by IOI Properties Group
IOI Properties Group has an exciting pipeline of upcoming projects. They are currently working on the development of new mixed-use developments, including residential, commercial, and hospitality components. The group is also exploring opportunities to expand their footprint internationally, aimed at bringing their expertise and innovative approach to real estate to new markets.
outlook for industrial and commercial property investment malaysia
3. SP Setia
An overview of SP Setia and its history
SP Setia is a renowned property developer that has made a significant mark on the Malaysian real estate landscape. Established in 1974, the company was initially focused on general contracting and construction. Over the years, SP Setia has grown into a leading property development company known for its commitment to quality, innovation, and sustainability.
Significant real estate projects undertaken by SP Setia
SP Setia has undertaken several significant real estate projects that have garnered praise and recognition. One of their notable developments is Setia Alam, a well-planned township that has become a benchmark for sustainable and community-centric living. The township features residential properties, commercial spaces, parks, schools, and a central business hub.
The influence of SP Setia on the Malaysian real estate market
SP Setia’s dedication to creating sustainable, liveable communities has had a tremendous influence on the Malaysian real estate market. Their developments prioritize green spaces, walkability, and connectivity, setting new standards for urban planning. The company’s efforts have not only improved the quality of life for residents but have also contributed to the overall development and growth of the surrounding areas.
Future plans and prospects of SP Setia
SP Setia has ambitious plans for the future. They are currently working on expanding their presence internationally, with a focus on markets such as Australia, Singapore, and the United Kingdom. The company also has several upcoming projects in the pipeline, including new residential and commercial developments that aim to redefine urban living in Malaysia.
4. EcoWorld Development Group
Introduction to EcoWorld Development Group
EcoWorld Development Group is a prominent real estate developer that has made a name for itself in Malaysia. Established in 2011, the company has quickly risen to prominence with its focus on sustainability, innovation, and community-centric development. EcoWorld is committed to creating developments that harmonize with the natural environment and enhance the well-being of its residents.
Noteworthy real estate developments by EcoWorld
EcoWorld’s portfolio includes several noteworthy real estate developments that have set new benchmarks in the industry. One of their standout projects is EcoCity, an integrated development that encompasses residential, commercial, and recreational components. The development is designed to promote sustainable living and features green spaces, bike-friendly infrastructure, and energy-efficient buildings.
EcoWorld’s impact on the Malaysian real estate industry
EcoWorld’s commitment to sustainability and community building has had a significant impact on the Malaysian real estate industry. Their developments have raised the bar for environmentally-friendly practices and have demonstrated the value of creating spaces that prioritize the well-being of residents. Additionally, EcoWorld’s emphasis on fostering a sense of community has helped create vibrant and cohesive neighborhoods.
Upcoming projects and initiatives by EcoWorld Development Group
EcoWorld has several exciting projects and initiatives in the pipeline. They are currently working on expanding their portfolio of mixed-use developments, including residential, commercial, and hospitality properties. The company is also exploring opportunities to incorporate smart technologies and green innovations into their projects, further enhancing the sustainability and livability of their developments.

5. Gamuda Land
Overview of Gamuda Land as a prominent developer
Gamuda Land is a renowned real estate developer in Malaysia, known for its commitment to innovation, quality, and sustainability. With a focus on creating vibrant, integrated communities, Gamuda Land has garnered accolades for its unique approach to development. The company has successfully delivered high-profile projects that have transformed the urban landscape.
Key real estate projects completed by Gamuda Land
Gamuda Land’s portfolio includes several key real estate projects that have shaped the Malaysian real estate scene. One of their iconic developments is Kota Kemuning, a township that has become a benchmark for sustainable living. The township features residential properties, commercial spaces, parks, and recreational facilities that cater to the needs of its residents.
The contribution of Gamuda Land to the Malaysian market
Gamuda Land has made significant contributions to the Malaysian real estate market. Their developments emphasize sustainability, incorporating green building practices, and promoting energy efficiency. These efforts have not only raised awareness about the importance of environmentally-friendly development but have also contributed to the overall well-being of residents and the surrounding communities.
Exciting upcoming ventures from Gamuda Land
Gamuda Land has several exciting projects in the pipeline. They are currently working on the development of new townships, mixed-use developments, and transit-oriented developments. The company is committed to continuously pushing boundaries and introducing innovative concepts that will shape the future of the Malaysian real estate industry.
6. Mah Sing Group
Introduction to Mah Sing Group and its background
Mah Sing Group is a prominent real estate developer in Malaysia with a history of over 25 years. The company has established itself as a reputable player in the industry, delivering high-quality residential, commercial, and industrial projects. Mah Sing Group is known for its focus on affordability, innovation, and customer satisfaction.
Prominent real estate projects delivered by Mah Sing Group
Mah Sing Group has successfully delivered several prominent real estate projects that have left a significant impact. One of their notable developments is Southville City, a township that offers a range of residential properties, commercial spaces, and recreational facilities. The township combines affordability with quality, catering to the needs of a diverse range of buyers.
The influence of Mah Sing Group on the Malaysian real estate scene
Mah Sing Group has had a notable influence on the Malaysian real estate scene. Their commitment to affordability has made homeownership more accessible to a wider audience, especially first-time buyers. Additionally, their focus on innovation and quality has contributed to the enhancement of the overall real estate market in Malaysia.
Future developments and plans of Mah Sing Group
Mah Sing Group has ambitious plans for the future. They are currently exploring opportunities to expand their presence internationally, aiming to bring their expertise and successful business model to new markets. The company also has several upcoming projects in strategic locations across Malaysia, catering to the growing demand for affordable and well-designed properties.

7. UEM Sunrise
An overview of UEM Sunrise and its journey
UEM Sunrise is a leading real estate developer that has played a significant role in shaping the Malaysian property market. The company was formed in 2008 through a merger between UEM Land and Sunrise Berhad. With a diverse portfolio of residential, commercial, and mixed-use developments, UEM Sunrise has become synonymous with quality and sustainability.
Key real estate developments undertaken by UEM Sunrise
UEM Sunrise has undertaken several key real estate developments that have become landmarks in Malaysia. One of their notable projects is Iskandar Puteri, a thriving township located in Johor. The township offers a mix of residential properties, educational institutions, retail outlets, and recreational amenities, creating a holistic living experience.
UEM Sunrise’s contributions to the Malaysian real estate market
UEM Sunrise has made significant contributions to the Malaysian real estate market, particularly in the area of sustainable development. The company has prioritized green building practices, connectivity, and community-building in their developments. They have also actively participated in urban regeneration projects, revitalizing existing spaces and transforming them into vibrant communities.
Upcoming projects and future prospects of UEM Sunrise
UEM Sunrise has a promising lineup of upcoming projects. They are currently working on the development of new residential, commercial, and mixed-use properties in strategic locations across Malaysia. The company is also exploring opportunities to expand their presence in international markets, aiming to bring their expertise and commitment to sustainability to new audiences.
8. S P Setia
Introduction to S P Setia and its history
S P Setia is a prominent Malaysian property developer that has made a significant impact on the real estate industry. Established in 1974, the company has built a reputation for its commitment to quality, innovation, and sustainability. S P Setia has an extensive portfolio of residential, commercial, and mixed-use developments that have played a crucial role in shaping the Malaysian property landscape.
Significant real estate projects completed by S P Setia
S P Setia has completed several significant real estate projects that have gained recognition and praise. One of their notable developments is Setia Alam, a well-planned township that has become a benchmark for sustainable living. The township offers a range of residential properties, commercial spaces, parks, schools, and community facilities.
The influence of S P Setia on the Malaysian market
S P Setia’s commitment to sustainable development and creating vibrant communities has had a significant influence on the Malaysian real estate market. Their developments prioritize green spaces, connectivity, and community-centric design, enhancing the quality of life for residents. The company has also contributed to the economic growth and development of the surrounding areas.
Future plans and prospects of S P Setia
S P Setia has exciting plans for the future. The company is exploring new opportunities to expand their presence in international markets, bringing their expertise and innovative approach to real estate to new audiences. Additionally, they have several upcoming projects in the pipeline, including new residential and commercial developments that will further enhance the possibilities for sustainable living in Malaysia.

9. Paramount Property
An overview of Paramount Property as a leading developer
Paramount Property is a leading real estate developer in Malaysia known for its commitment to quality, innovation, and customer satisfaction. The company has a diverse portfolio of residential, commercial, and educational developments. Paramount Property is dedicated to creating exceptional living and working spaces that meet the needs of a wide range of customers.
Key real estate projects completed by Paramount Property
Paramount Property has successfully completed several key real estate projects that have become prominent landmarks. One of their notable developments is Sejati Residences, a luxury residential development that offers exclusive and spacious homes. The development combines modern designs with green spaces, creating a harmonious living environment.
The impact of Paramount Property on the Malaysian real estate industry
Paramount Property has had a significant impact on the Malaysian real estate industry. Their developments have raised the bar for quality and innovation, setting new standards for modern living. The company’s commitment to sustainability and green practices has also contributed to the overall well-being of residents and the surrounding communities.
Exciting future ventures from Paramount Property
Paramount Property has several exciting future ventures in the pipeline. They are currently working on the development of new residential and commercial projects that cater to the evolving needs of the market. The company is also exploring opportunities to incorporate smart technologies and sustainable design principles into their developments, creating spaces that are future-ready.
10. IJM Land
Introduction to IJM Land and its background
IJM Land is a prominent real estate developer in Malaysia, with a rich history and a diverse portfolio of residential, commercial, and industrial properties. The company is known for its commitment to quality, innovation, and sustainable development. IJM Land’s projects are designed to meet the needs of a wide range of customers, from first-time homebuyers to established businesses.
Noteworthy real estate developments by IJM Land
IJM Land has delivered several noteworthy real estate developments that have become landmarks in Malaysia. One of their standout projects is Pantai Sentral Park, an integrated development that offers a mix of residential, commercial, and recreational components. The development is designed to promote a healthy and balanced lifestyle, incorporating green spaces and wellness amenities.
The influence of IJM Land on the Malaysian real estate scene
IJM Land has made a significant impact on the Malaysian real estate scene. Their developments prioritize quality and sustainability, setting new benchmarks for modern living. The company has actively contributed to the growth and development of the communities in which they operate, creating vibrant and cohesive neighborhoods.
Future projects and plans of IJM Land
IJM Land has ambitious plans for the future. They are currently working on expanding their portfolio of residential, commercial, and mixed-use developments. The company is committed to incorporating sustainable design principles and green technologies into their projects, creating spaces that are not only aesthetically pleasing but also environmentally friendly and energy-efficient.
Exploring the Power of Context-Aware Virtual Assistant Responses
If you’ve ever wondered just how powerful context-aware virtual assistant responses can be, then this article is for you. We’ll be exploring the fascinating world of AI assistants and how they are becoming more adept at understanding and responding to human context. From embedding videos to using proper alt text, these virtual assistants are pulling out all the stops to provide a friendly and engaging user experience. So get ready to be amazed by the incredible capabilities of context-aware virtual assistant responses.
1. What are Context-Aware Virtual Assistant Responses?
1.1 Definition
Context-Aware Virtual Assistant Responses refer to the intelligent and adaptive replies generated by virtual assistants, such as Siri, Alexa, Google Assistant, Cortana, and IBM Watson Assistant, based on the understanding of user context. These responses are designed to provide personalized and relevant information to users, considering factors such as their previous interactions, location, preferences, and current situation.
1.2 Importance
Context-Aware Virtual Assistant Responses have gained significant importance in recent years due to the growing demand for personalized and efficient virtual assistant services. By understanding the context in which users interact with virtual assistants, these responses can deliver more accurate and helpful information, resulting in an enhanced user experience. They also play a crucial role in increasing the efficiency of virtual assistants by automating processes and reducing the need for repetitive queries. Moreover, context-aware responses enable virtual assistants to adapt to individual users, delivering a personalized interaction that feels more natural and intuitive.
2. How Context-Aware Virtual Assistant Responses Work
2.1 Understanding Context
To generate context-aware responses, virtual assistants utilize sophisticated algorithms and technologies to understand various dimensions of user context. This includes gathering information about the user’s identity, preferences, past behaviors, location, and current situation. By analyzing these contextual factors, virtual assistants can tailor their responses to provide accurate and relevant information.
2.2 Gathering and Analyzing Data
Context-aware virtual assistants rely on a vast amount of data to understand the user’s context. This data is collected from various sources, such as user profiles, device sensors, and historical data. For example, virtual assistants may collect data about a user’s previous interactions, browsing history, and purchase behavior. This data is then analyzed to extract meaningful patterns and insights to guide the generation of appropriate responses.
2.3 Natural Language Processing
Natural Language Processing (NLP) is a key component of context-aware virtual assistant responses. NLP enables virtual assistants to understand and interpret user queries in a human-like manner. By leveraging techniques like speech recognition and semantic analysis, virtual assistants can accurately comprehend the nuances of language, allowing them to generate contextually relevant responses.
2.4 Machine Learning
Machine Learning algorithms play a vital role in enabling virtual assistants to adapt and improve their responses over time. These algorithms analyze historical data and user feedback to learn patterns and trends, enabling virtual assistants to make more accurate predictions about user preferences and context. Through continuous learning, virtual assistants can refine their response generation process and deliver increasingly personalized and relevant information.
2.5 Response Generation
Once the user’s context has been understood and analyzed, virtual assistants generate appropriate responses using a combination of pre-defined templates and dynamic content. These responses can range from simple factual answers to complex recommendations and explanations. Virtual assistants may also use natural language generation techniques to ensure the responses sound natural and coherent. The generated response is then presented to the user through text or speech, depending on the interaction medium.
3. Benefits of Context-Aware Virtual Assistant Responses
3.1 Enhanced User Experience
Context-aware virtual assistant responses significantly enhance the overall user experience by delivering personalized and relevant information. By understanding user preferences and adapting to individual contexts, virtual assistants can provide more accurate and helpful responses. This results in a more intuitive and efficient interaction, saving users time and effort.
3.2 Increased Efficiency
By leveraging context-aware responses, virtual assistants can automate processes and handle user queries more efficiently. For example, a virtual assistant can anticipate user needs by analyzing previous interactions and proactively provide relevant information. This automation reduces the need for repetitive queries and speeds up the overall interaction, improving efficiency for both users and businesses.
3.3 Personalized Interactions
Context-aware virtual assistant responses enable personalized interactions that cater to individual user preferences. By considering factors such as user history, location, and preferences, virtual assistants can deliver recommendations, suggestions, and content tailored to each user’s unique needs. This personalization creates a more engaging and customized experience for users, fostering a stronger connection with the virtual assistant.
3.4 Reduced Errors and Frustration
With context-aware responses, virtual assistants can reduce errors and frustration by providing accurate and relevant information. By understanding the user’s context, virtual assistants can avoid misunderstandings and deliver more precise responses. This reduces the likelihood of errors or misleading information, resulting in a more satisfactory user experience.
4. Challenges and Limitations
4.1 Privacy and Security Concerns
Context-aware virtual assistant responses heavily rely on collecting and analyzing user data, raising concerns around privacy and security. Users may feel uneasy about the extent of information collected and how it is used. Companies must ensure transparent data practices, robust security measures, and obtain explicit consent from users before gathering and analyzing their data to address these concerns.
4.2 Dependency on Accurate Data
The accuracy of context-aware virtual assistant responses heavily depends on the quality of the data used for analysis. If inaccurate or incomplete data is used, virtual assistants may generate incorrect or irrelevant responses. It is essential to have reliable data sources and regular data validation processes in place to mitigate this challenge.
4.3 Cultural and Linguistic Variations
Context-aware virtual assistant responses may face challenges in understanding and adapting to cultural and linguistic variations. Different languages, dialects, and cultural nuances can impact the accuracy and relevance of responses. Developers must consider these variations and invest in fine-tuning their algorithms to ensure context-aware responses are effective across diverse cultural and linguistic backgrounds.
4.4 Ethical Considerations
The generation of context-aware responses raises ethical considerations, especially regarding bias and discrimination. Virtual assistant algorithms must be designed to prevent biases based on factors like race, gender, or socioeconomic status. Transparency in the response generation process is crucial to mitigate these ethical concerns and ensure fair and unbiased interactions.

5. Use Cases of Context-Aware Virtual Assistant Responses
5.1 Customer Service
Context-aware virtual assistant responses have significant applications in customer service. Virtual assistants can analyze user context to understand their needs and provide personalized support, such as product recommendations, troubleshooting assistance, and order tracking. This enhances the customer service experience by delivering timely, accurate, and relevant information, ultimately boosting customer satisfaction.
5.2 Healthcare
In the healthcare sector, context-aware virtual assistant responses can assist patients with personalized guidance and support. Virtual assistants can collect and analyze patient data to provide medication reminders, symptom assessment, and general health advice. By understanding individual health contexts, virtual assistants can offer targeted recommendations and assist in healthcare management.
5.3 E-commerce
Context-aware virtual assistant responses have valuable applications in the e-commerce industry. Virtual assistants can analyze user browsing history, purchase behavior, and preferences to offer personalized product recommendations, assist in the buying process, and provide detailed product information. This personalized approach enhances the customer shopping experience, leading to increased conversions and customer loyalty.
5.4 Smart Homes
Context-aware virtual assistant responses can enhance the functionality of smart home systems. By understanding user preferences, location, and daily routines, virtual assistants can control various devices and automate routine tasks, such as adjusting temperature, turning on lights, or playing music. This improves convenience and energy efficiency, creating a seamless and personalized home environment.
5.5 Travel and Tourism
Virtual assistants can provide valuable support in the travel and tourism industry by offering context-aware responses. By understanding user travel plans, preferences, and location, virtual assistants can suggest personalized itineraries, provide real-time weather updates, recommend local attractions, and assist with booking flights and accommodations. This enhances the travel experience and provides users with tailored information to make the most of their trips.
6. Context-Aware Virtual Assistant Response Platforms
6.1 Amazon Alexa
Amazon Alexa is one of the leading context-aware virtual assistant platforms. It leverages advanced NLP and machine learning algorithms to understand user queries and generate contextually relevant responses. With a vast ecosystem of skills and integrations, Amazon Alexa can provide personalized information, control smart devices, and assist in various domains, such as entertainment, household management, and shopping.
6.2 Google Assistant
Google Assistant is another prominent context-aware virtual assistant platform. Developed by Google, it utilizes powerful natural language understanding capabilities to interpret user queries and generate accurate responses. Google Assistant is seamlessly integrated into various devices and services, providing personalized assistance across multiple domains, including search, productivity, smart home control, and entertainment.
6.3 Apple Siri
Apple Siri is a well-known context-aware virtual assistant available on Apple devices. Siri combines speech recognition, language processing, and machine learning to understand user queries and provide relevant responses. Siri integrates with Apple’s ecosystem, allowing users to interact with various services, such as messaging, navigation, reminders, and music, using voice commands.
6.4 Microsoft Cortana
Microsoft Cortana is a context-aware virtual assistant developed by Microsoft. Cortana utilizes advanced algorithms to understand user context, preferences, and habits. It provides personalized information, recommendations, and assistance across multiple platforms, including Windows devices, Microsoft Office, and other compatible applications.
6.5 IBM Watson Assistant
IBM Watson Assistant is a robust and versatile context-aware virtual assistant platform. It leverages powerful AI technologies, including natural language processing and machine learning, to understand and respond to user queries. Watson Assistant can be customized to meet specific business needs and is widely adopted in various industries, such as healthcare, banking, and customer support.
7. Future Trends and Innovations
7.1 Natural Language Understanding Advancements
In the future, context-aware virtual assistant responses will continue to evolve with advancements in natural language understanding. Virtual assistants will become more proficient in understanding and interpreting complex user queries, including conversational and contextual nuances. This will enhance the accuracy and relevance of responses, providing users with more comprehensive and helpful information.
7.2 Emotion and Sentiment Analysis
An emerging trend in context-aware virtual assistant responses is the integration of emotion and sentiment analysis. Virtual assistants will be able to detect and interpret user emotions based on voice tone, facial expressions, and language patterns. This will enable virtual assistants to respond empathetically and appropriately in various situations, further improving the user experience.
7.3 Integration with Internet of Things (IoT)
Context-aware virtual assistant responses will increasingly be integrated with the Internet of Things (IoT) ecosystem. Virtual assistants will be able to control and interact with a wide range of IoT devices, such as smart thermostats, security systems, and appliances, to provide users with seamless and personalized home automation experiences.
7.4 Voice Biometrics
Voice biometrics is an emerging technology that can add a layer of security and personalization to context-aware virtual assistant responses. By analyzing unique voice characteristics, virtual assistants can verify user identity and tailor responses based on individual preferences. Voice biometrics can enhance the security of virtual assistant interactions and deliver a more personalized experience.
7.5 Context-Aware Actions
Future advancements in context-aware virtual assistant responses will focus on enabling virtual assistants to take context-aware actions. Virtual assistants will be able to initiate actions on behalf of the user, such as ordering products, scheduling appointments, or making reservations, based on their understanding of user context. This will further automate tasks and provide users with a more seamless and hands-free experience.
8. Ethical Considerations in Context-Aware Virtual Assistant Responses
8.1 Privacy and Data Protection
As context-aware virtual assistant responses rely on collecting and analyzing user data, it is crucial to address privacy and data protection concerns. Companies must implement robust security measures to safeguard user information and provide transparent data practices. Users should have control over their data and the ability to manage its usage by virtual assistants.
8.2 Transparency and Accountability
Virtual assistant platforms should strive for transparency and accountability in their response generation processes. Users should be informed about how virtual assistants analyze their data and generate responses. Clear guidelines and policies should be in place to address any concerns related to bias, discrimination, or misuse of user data. Regular audits and external oversight can help ensure accountability.
8.3 Bias and Discrimination
Context-aware virtual assistant responses should be designed to mitigate biases and avoid discrimination. Developers must ensure that algorithms are trained on diverse and representative datasets to prevent biases related to race, gender, or socioeconomic status. Regular monitoring and auditing should be done to identify and rectify any potential biases in the response generation process.

9. Conclusion
Context-Aware Virtual Assistant Responses have transformed the way users interact with virtual assistants, providing personalized and relevant information based on user context. By understanding factors such as user preferences, location, and past behaviors, context-aware responses enhance user experience, increase efficiency, and enable personalized interactions. Although challenges like privacy concerns, data accuracy, and cultural variations exist, the benefits of context-aware virtual assistant responses are significant, impacting various industries such as customer service, healthcare, e-commerce, smart homes, and travel. As technology advances, future trends and innovations will further enhance the capabilities of context-aware virtual assistants, incorporating natural language understanding advancements, emotion analysis, IoT integration, voice biometrics, and context-aware actions. However, ethical considerations regarding privacy, transparency, accountability, and bias must be carefully addressed to ensure responsible and fair use of context-aware virtual assistant responses.


The Ultimate Guide to Choosing the Top Vacuum Cleaner in Malaysia
Looking for the perfect vacuum cleaner in Malaysia? Look no further! In this ultimate guide, we’ll walk you through everything you need to know to make an informed decision. From understanding the different types of vacuum cleaners to helpful tips on what features to prioritize, we’ve got you covered. With proper headings, engaging content, and visual aids like videos and images, this friendly article aims to captivate your interest and provide you with all the information you need to choose the top vacuum cleaner for your needs in Malaysia. Say goodbye to dust and dirt, and say hello to a cleaner home!
Factors to Consider Before Buying a Vacuum Cleaner
When it comes to buying a vacuum cleaner, there are several factors you should consider to ensure you make the right choice for your cleaning needs. From the type of vacuum cleaner to the accessories and attachments, each element can have a significant impact on performance and functionality. By understanding these factors, you’ll be able to make an informed decision and find the perfect vacuum cleaner for your home or office. Let’s dive into each factor in detail.
Type of Vacuum Cleaner
The first factor to consider is the type of vacuum cleaner that best suits your needs. There are several types to choose from, each with its own strengths and weaknesses. Here are the most common types of vacuum cleaners you’ll come across:
Upright Vacuum Cleaners
Upright vacuum cleaners are the classic choice for many households. They are versatile and typically feature a rotating brush roll for effective carpet cleaning. With their upright design, they are easy to maneuver and offer excellent suction power.
Canister Vacuum Cleaners
Canister vacuums consist of a separate canister unit connected to a wand and cleaning head by a hose. They are known for their versatility and maneuverability, making them great for cleaning tight spaces and stairs. Canister vacuums often offer powerful suction and come with a variety of attachments for different cleaning tasks.
Stick Vacuum Cleaners
Stick vacuum cleaners are lightweight and slender, making them perfect for quick and easy cleaning. They are ideal for smaller spaces and surface cleaning, but may not have the same level of suction power as upright or canister vacuums.
Robot Vacuum Cleaners
Robot vacuum cleaners are the ultimate hands-free cleaning solution. They can navigate around your home autonomously, cleaning various surfaces such as carpets and hard floors. Robot vacuums are perfect for busy individuals who want to maintain a clean home without putting in too much effort.
Handheld Vacuum Cleaners
Handheld vacuum cleaners are compact and portable, making them excellent for cleaning small messes or reaching tight spaces. They are perfect for quick clean-ups and spot cleaning.
Convertible Vacuum Cleaners
Convertible vacuum cleaners offer the flexibility to convert between different configurations. For example, they can be used as both an upright and a canister vacuum. This versatility allows you to adapt the vacuum cleaner to different cleaning tasks and spaces.
Before purchasing a vacuum cleaner, consider the type that will best suit your cleaning needs. Think about the size of your home, the type of flooring you have, and the specific cleaning tasks you’ll be performing.

Suction Power
Another crucial factor to consider is the suction power of the vacuum cleaner. Suction power determines how effectively the vacuum can pick up dirt, debris, and pet hair. A vacuum cleaner with high suction power will ensure thorough cleaning and leave your floors spotless.
Understanding Suction Power
Suction power is usually measured in air watts or cubic feet per minute (CFM). Air watts measure the vacuum cleaner’s overall power, while CFM measures the volume of airflow produced. Look for a vacuum cleaner with high air watts or CFM ratings for optimal suction power.
Consideration for Different Floor Types
Different flooring surfaces require different levels of suction power. For carpets, a vacuum cleaner with a strong suction and a rotating brush roll can effectively remove embedded dirt and dust. On the other hand, hard floors may require a vacuum cleaner with adjustable suction settings to prevent scattering debris.
Pet Hair and Allergen Removal
If you have pets or suffer from allergies, choosing a vacuum cleaner with specialized features for pet hair and allergen removal is essential. Look for models with powerful suction and effective filtration systems to eliminate pet hair and allergens from your home.
Effectiveness on Carpets and Rugs
Carpets and rugs often trap dust, dirt, and allergens deep within their fibers. When selecting a vacuum cleaner, consider its ability to deep-clean carpets and effectively remove embedded particles.
Performance on Hard Floors
For hard floors, such as laminate, hardwood, or tile, you’ll want a vacuum cleaner that can efficiently pick up debris without scratching the surface. Look for models with soft brushes or attachments specifically designed for hard floors.
When assessing the suction power of a vacuum cleaner, consider your specific cleaning needs, the types of surfaces in your home, and any unique challenges like pet hair or allergies.
Bagged vs Bagless Vacuum Cleaners
The next factor to consider is whether you prefer a bagged or bagless vacuum cleaner. Both options have their advantages and disadvantages, so understanding the pros and cons will help you make an informed decision.
Pros and Cons of Bagged Vacuum Cleaners
Bagged vacuum cleaners use disposable bags to collect dirt and debris. Here are some pros and cons to consider:
Pros
- Hygienic disposal: Bagged vacuum cleaners can offer a more hygienic disposal process since you can simply remove the bag and throw it away without any contact with the dirt or allergens.
- Less mess during emptying: Bagged vacuum cleaners minimize the chances of debris spilling out during the emptying process.
- Higher dust capacity: Bagged models often have larger dust capacities, allowing you to clean for longer periods without needing to empty the bag.
Cons
- Ongoing cost: Bagged vacuum cleaners require regular replacement of the bags, which can add to the overall cost.
- Reduced suction as bag fills: As the bag fills up, the suction power may decrease, requiring you to replace the bag more frequently.
- Limited visibility: Since the dirt is contained within the bag, it may be challenging to see how full the bag is without opening the vacuum cleaner.
Pros and Cons of Bagless Vacuum Cleaners
Bagless vacuum cleaners use dust containers or canisters to collect dirt and debris. Here are some pros and cons to consider:
Pros
- Cost-effective in the long run: Bagless vacuum cleaners eliminate the need to purchase replacement bags, reducing ongoing costs.
- Ease of emptying: With bagless models, you can easily remove the dust container, empty it, and return it to the vacuum cleaner.
- Visible dust capacity: Bagless models often come with transparent canisters, allowing you to see when it’s time to empty the container.
Cons
- Messy emptying process: Emptying a bagless vacuum cleaner can be messy, especially if you suffer from allergies or sensitivity to dust.
- Regular filter cleaning: Most bagless models require regular cleaning of filters to maintain optimal performance and prevent clogging.
- Smaller dust capacity: Bagless vacuum cleaners typically have smaller dust capacities compared to their bagged counterparts, meaning you may need to empty them more frequently.
Consider your personal preference and cleaning habits when deciding between bagged and bagless vacuum cleaners.
best cordless vacuum cleaner malaysia
Filtration Systems
A vacuum cleaner’s filtration system plays a crucial role in maintaining indoor air quality and trapping allergens. There are several types of filtration systems to consider when choosing a vacuum cleaner.
High-Efficiency Particulate Air (HEPA) Filters
HEPA filters are considered the gold standard in filtration systems. They can capture up to 99.97% of particles as small as 0.3 microns, including dust mites, pollen, pet dander, and other allergens. If you or your family members suffer from allergies or asthma, choosing a vacuum cleaner with a HEPA filter is highly recommended.
Cyclonic Filtration
Cyclonic filtration systems use centrifugal force to separate dirt and debris from the airflow. They are effective in preventing clogs and maintaining suction power. While not as efficient as HEPA filters in capturing fine particles, cyclonic filtration systems can still provide good overall filtration.
Water Filtration
Water filtration is an innovative filtration system that uses water to capture dust and allergens. The dirt and debris are trapped in the water, preventing them from being released back into the air. Vacuum cleaners with water filtration can be an excellent choice for individuals with severe allergies or asthma.
Consider the filtration system of a vacuum cleaner to ensure it effectively captures dust, allergens, and other particles, providing cleaner air during the cleaning process.
Size and Weight Considerations
The size and weight of a vacuum cleaner can greatly impact its maneuverability and usability. Consider the following factors when evaluating the size and weight of a vacuum cleaner:
Maneuverability and Storage
A lightweight and compact vacuum cleaner is easier to maneuver around furniture, corners, and tight spaces. If you have multiple levels in your home or struggle with mobility, a lightweight vacuum cleaner will make it easier to clean hard-to-reach areas and carry between floors. Additionally, consider the storage space available in your home and choose a vacuum cleaner that can be stored conveniently.
Stair and Upholstery Cleaning
If you have stairs or frequently need to clean upholstery, consider a vacuum cleaner with specific features for these tasks. Look for models with detachable handheld units or specialized attachments for stair cleaning and removing pet hair from upholstery.
User Mobility
If you or someone in your household has limited mobility or strength, a lightweight vacuum cleaner with ergonomic handles and maneuverable swivel heads will be more user-friendly. Ensure the vacuum cleaner is easy to push, pull, and steer to prevent fatigue or strain during use.
By considering the size and weight of a vacuum cleaner, you can choose one that is comfortable to handle and suits your individual cleaning needs.
cordless vacuum cleaner malaysia
Noise Level
The noise level of a vacuum cleaner can greatly affect your cleaning experience, especially if you have young children, pets, or live in an apartment building. Here are some factors to consider when evaluating the noise level of a vacuum cleaner:
Decibel Ratings
Decibel (dB) ratings indicate the noise level produced by a vacuum cleaner. Lower dB ratings indicate quieter operation, while higher dB ratings suggest a louder machine. Look for vacuum cleaners with lower dB ratings if noise is a concern in your household.
Noise Reduction Technology
Some vacuum cleaners come equipped with noise reduction technology to minimize the sound they produce. These models often have sound-dampening insulation or special design features that reduce vibrations and noise levels during operation.
Consideration for Different Environments
If you live in an apartment or have neighbors in close proximity, consider choosing a vacuum cleaner with a quieter operation to avoid disturbing others. Additionally, if you have babies or young children who are sensitive to loud noises, a quieter vacuum cleaner will make cleaning sessions more enjoyable for them.
Prioritize your comfort and the peace of your household when selecting a vacuum cleaner with a noise level that suits your needs.
Corded vs Cordless Vacuum Cleaners
The choice between a corded or cordless vacuum cleaner depends on your cleaning preferences and lifestyle. Consider the following factors when deciding between the two options:
Convenience and Portability
Cordless vacuum cleaners offer unmatched convenience and portability. They allow you to move freely without the restrictions of a power cord, making it easier to clean multiple rooms or hard-to-reach areas. Cordless vacuum cleaners are ideal for quick clean-ups or if you have limited power outlets in your home.
On the other hand, corded vacuum cleaners offer continuous power without the need to recharge batteries. They are typically more powerful and suitable for deep cleaning larger areas. Corded models are well-suited for individuals who prefer longer cleaning sessions and don’t want to worry about battery life.
Battery Life and Charging Time
If you opt for a cordless vacuum cleaner, it’s essential to consider the battery life and charging time. Look for models with longer battery life, especially if you have a larger home or multiple floors to clean. Additionally, consider the charging time required to fully recharge the batteries, as some models may take several hours to reach a full charge.
Suction Power Comparison
Corded vacuum cleaners generally offer more suction power compared to cordless models. If you have dense carpets or heavily soiled areas that require deep cleaning, a corded vacuum cleaner may provide the necessary power. Cordless models, while convenient, may not have the same level of suction and may struggle with tougher cleaning tasks.
Consider your cleaning routine, the size of your home, and the specific cleaning challenges you face when deciding between a corded or cordless vacuum cleaner.

Accessories and Attachments
The availability and quality of accessories and attachments can greatly enhance the functionality and versatility of a vacuum cleaner. Here are some key considerations when evaluating the accessories and attachments:
Common Accessories
Most vacuum cleaners come with standard accessories, such as crevice tools, dusting brushes, and upholstery attachments. These attachments are handy for cleaning hard-to-reach areas, dusting furniture and shelves, and removing pet hair from upholstery.
Specialized Attachments
Consider any specific cleaning tasks you frequently encounter and choose a vacuum cleaner that offers specialized attachments to address those needs. For example, if you have a lot of pet hair, look for a model with a pet brush attachment. If you have delicate surfaces like wood or glass, consider a vacuum cleaner with a soft brush attachment to prevent scratches.
Ease of Attachment and Removal
Evaluate how easy it is to attach and remove the accessories. A vacuum cleaner with a quick-release feature will make it more convenient to switch between attachments and adapt to different cleaning tasks.
The availability and quality of accessories and attachments can significantly enhance the versatility and effectiveness of a vacuum cleaner. Consider your specific cleaning needs and choose a model that comes with the accessories that will be most useful to you.
Warranty and Customer Support
The warranty and customer support provided by the vacuum cleaner manufacturer can give you peace of mind and assurance of quality. Here are some factors to consider:
Warranty Coverage
Check the warranty coverage offered by the manufacturer. Look for a vacuum cleaner that comes with at least a one-year warranty, as this ensures that any defects or malfunctions will be taken care of within a reasonable timeframe.
Customer Support
Research the reputation of the manufacturer’s customer support. Read customer reviews and check if there are any common complaints regarding the manufacturer’s responsiveness and willingness to assist with troubleshooting or repairs.
Return Policies
Understand the return policies and procedures in case you encounter any issues with the vacuum cleaner. Ensure that the manufacturer or retailer has a hassle-free return process in the rare event that you are unsatisfied with your purchase.
Choosing a vacuum cleaner from a reputable manufacturer with a solid warranty and reliable customer support will provide you with peace of mind and ensure a positive ownership experience.

Price Range
The last factor to consider before buying a vacuum cleaner is the price range that fits within your budget. Vacuum cleaners are available at various price points, so it’s essential to determine how much you are willing to invest.
Budget Range
Set a realistic budget that suits your cleaning needs and financial situation. Consider the long-term value and performance of the vacuum cleaner rather than just the initial price. It’s worth investing in a quality vacuum cleaner that will serve you well for years to come.
Value for Money
When assessing a vacuum cleaner’s value for money, consider its features, performance, durability, and warranty coverage. A slightly more expensive model with better performance and a longer warranty may provide better value over time compared to a cheaper option.
Long-Term Cost Analysis
Apart from the initial purchase price, consider any ongoing costs associated with the vacuum cleaner. For example, bagged models require regular bag replacements, while bagless models may require filter replacements. Factor in these costs to get a complete picture of the long-term affordability of a vacuum cleaner.
By determining your budget range, evaluating the value for money, and considering the long-term costs, you can make a wise investment in a vacuum cleaner that aligns with your financial situation.
In conclusion, buying a vacuum cleaner requires careful consideration of various factors to ensure you make the right choice. Evaluate the type of vacuum cleaner that suits your needs, assess the suction power and performance, decide between bagged or bagless options, consider the filtration system, size and weight, noise level, corded or cordless functionality, available accessories and attachments, warranty and customer support, and price range. By taking these factors into account, you’ll be able to find the perfect vacuum cleaner that meets your cleaning requirements and helps maintain a clean and healthy environment in your home or office. Happy vacuuming!


AI in Education: Transforming Learning for the Digital Age
In the dynamic landscape of education, Artificial Intelligence (AI) emerges as a transformative force, revolutionizing traditional teaching methods and unlocking new possibilities for learners. As we explore the impact of AI in education, we delve into a world where technology becomes a catalyst for personalized learning, accessibility, and educational innovation.
Personalized Learning: Tailoring Education to Individual Needs AI in education paves the way for personalized learning experiences, catering to the unique needs and learning styles of each student. Adaptive learning platforms analyze student performance, offering targeted interventions and customizing curricula to ensure that education aligns with individual strengths and weaknesses.
Accessibility and Inclusivity: Bridging Gaps in Education One of the remarkable contributions of AI in education is its role in promoting accessibility and inclusivity. Intelligent tools assist students with diverse learning abilities, providing support in real-time. AI-powered language translation and transcription services break down language barriers, fostering a more inclusive educational environment.
Smart Classrooms: Revolutionizing the Teaching-Learning Paradigm The traditional classroom undergoes a metamorphosis with the integration of AI. Smart classrooms equipped with interactive whiteboards, AI-driven educational apps, and virtual simulations create an immersive learning experience. Teachers leverage AI tools to track student progress, identify areas for improvement, and tailor their teaching methods accordingly.
AI Tutors: Enhancing Learning Beyond the Classroom AI-powered tutoring systems act as virtual mentors, supplementing classroom instruction. These intelligent tutors offer additional support, answering queries, providing explanations, and adapting to the pace of individual learners. The result is a more dynamic and responsive learning environment that extends beyond traditional classroom hours.
Gamification of Learning: Making Education Engaging and Fun AI injects an element of gamification into education, transforming the learning process into an engaging and interactive experience. Educational games powered by AI algorithms captivate students’ interest, fostering a love for learning while simultaneously reinforcing key concepts in a playful and enjoyable with V circle.
Data-Driven Decision Making: Shaping Educational Strategies AI analytics in education enable data-driven decision-making at both the institutional and individual levels. Schools and educators can analyze vast datasets to identify trends, measure student performance, and optimize teaching methodologies. This data-driven approach empowers educators to make informed decisions that enhance overall educational outcomes.
Challenges and Ethical Considerations: Navigating the Educational AI Landscape While AI brings numerous benefits to education, it also raises ethical considerations and challenges. Issues such as data privacy, algorithmic bias, and the responsible use of AI tools require careful navigation. Striking a balance between innovation and ethical considerations is essential to ensure the positive impact of AI in education.
Conclusion: As AI transforms the educational landscape, it heralds a new era of learning that is personalized, inclusive, and technologically enriched. The integration of AI in education not only enhances the learning experience for students but also empowers educators to optimize their teaching strategies. As we navigate the evolving intersection of AI and education, the promise of a more accessible, engaging, and effective learning environment unfolds.


Cord Banking Benefits: Unlocking the Potential of Nature’s Precious Gift
Introduction:
Cord banking, a revolutionary medical practice, offers families an exceptional opportunity to harness the life-changing benefits of their newborn’s umbilical cord. By preserving the precious stem cells found within, cord banking opens doors to a multitude of potential health advantages for your child and loved ones. In this article, we will explore the wonders of cord banking benefits, delve into the science of stem cells, and highlight the significance of making an informed decision to secure a healthier and more resilient future.
Content:
1. Understanding Cord Banking: In this section, we’ll provide a comprehensive overview of cord banking and its profound impact on modern healthcare. Cord banking involves collecting and preserving the stem cells from a baby’s umbilical cord, which hold immense potential for treating various diseases and medical conditions.
2. The Miracle of Stem Cells: Delve into the fascinating realm of stem cells, nature’s regenerative powerhouses. We’ll uncover the incredible abilities of these versatile cells to repair and rejuvenate damaged tissues, contributing to the marvels of medical science and emphasizing the significance of cord banking.
3. Empowering Health with Cord Banking Benefits: This section will explore the numerous benefits of cord banking. From offering a genetically compatible source of stem cells to potentially treating leukemia, immune system disorders, and more, cord banking stands as a proactive investment in your family’s well-being.
4. Cord Banking Price: The Investment for a Healthier Tomorrow: In this segment, we’ll discuss the investment associated with cord banking and its tangible worth in securing your family’s health. By weighing the costs against the potential medical benefits, parents can make an informed decision that aligns with their budget and long-term health goals.
5. Private vs. Public Cord Banking: Making the Right Choice: Here, we’ll explore the options of private and public cord banking. Private cord banking ensures exclusive access to the stored stem cells for your family’s use, while public cord banking allows the cord blood to be donated for the benefit of others in need.
**6. Cord Banking: A Gift for Life: In this section, we’ll emphasize the lifelong advantages of cord banking. By preserving this precious gift of life, parents are providing their child and family members with a proactive resource that may prove invaluable in times of medical need.
Conclusion:
Cord banking benefits are a testament to the marvels of medical science and the wonders of nature. By preserving the potent stem cells found in umbilical cords, parents are gifting their children and loved ones with a source of regenerative potential that can transform lives. Making the decision to invest in cord banking is an empowering step towards securing a healthier and more resilient future for your family.
FAQs:
Q1. Are cord banking benefits only limited to the child? Answer: No, cord banking benefits extend beyond the child. The stored stem cells can potentially benefit immediate family members who may require a compatible match for medical treatments.
Q2. Can cord banking benefits be accessed at any age? Answer: Yes, cord banking preserves the stem cells at their most potent state, making them viable for potential medical use throughout a person’s life.
Q3. Is cord banking a guarantee for preventing diseases? Answer: While cord banking offers potential medical benefits, it cannot guarantee the prevention of diseases. However, it equips your family with a valuable resource that may aid in treatments if the need arises.
Q4. Can cord banking be considered an investment in my family’s health? Answer: Absolutely! Cord banking is an investment in your family’s health and well-being, offering a proactive approach to future medical challenges.
Q5. Can cord banking benefits be accessed in public cord banks? Answer: Public cord banks provide the opportunity to donate cord blood for the benefit of others in need. For exclusive access to the stored stem cells, private cord banking is recommended.

Umbilical Cord Blood Banking: A Wise Investment in Your Child’s Health
Umbilical cord blood banking is a forward-thinking medical practice that offers parents the opportunity to secure a precious resource with potential life-saving benefits. The umbilical cord, once considered medical waste, is now recognized for its rich source of valuable stem cells. These stem cells have the remarkable ability to regenerate and repair damaged tissues, making them invaluable for treating various diseases and medical conditions. In this article, we will delve into the significance of umbilical cord blood banking, the process involved, the advantages it offers, and the importance of informed decision-making for your child’s future health.
The Importance of Umbilical Cord Blood Banking
Unlocking the Potential of Stem Cells:
The umbilical cord blood contains hematopoietic stem cells, which can transform into different types of blood cells. These versatile cells have shown immense potential in medical treatments, revolutionizing the field of regenerative medicine.
A Non-Invasive Procedure:
Umbilical cord blood banking is a simple and non-invasive procedure that poses no risk or harm to the baby or the mother. The cord blood is collected after the baby’s birth, making it a safe and ethical source of stem cells.
The Process of Umbilical Cord Blood Banking
Collection:
Immediately after childbirth and the clamping of the umbilical cord, the remaining blood in the cord is collected using a sterile collection kit. This process takes only a few minutes and does not interfere with the birthing experience.
Testing and Processing:
The collected cord blood is sent to a specialized laboratory for testing and processing. The stem cells are isolated, and the cord blood is screened for infections and other factors to ensure its suitability for preservation.
Cryopreservation:
After processing, the stem cells are cryopreserved or frozen at ultra-low temperatures to maintain their viability and potency over time. Cryopreservation ensures that the stem cells remain intact and ready for potential future use.
The Advantages of Umbilical Cord Blood Banking
1. Medical Insurance for Your Child:
Umbilical cord blood banking is like a medical insurance policy for your child’s health. By preserving the stem cells, you are providing a valuable resource that may be crucial in treating unforeseen medical conditions in the future.
2. Compatibility Advantage:
The stem cells in umbilical cord blood are a perfect genetic match for the baby from whom they are collected. This compatibility increases the chances of successful transplants and reduces the risk of rejection.
3. Treatment of Blood Disorders:
Umbilical cord blood stem cells have proven effective in the treatment of various blood disorders, including leukemia, lymphoma, and sickle cell anemia. They can restore the blood and immune system, offering hope to patients with these conditions.
4. Advancements in Regenerative Therapies:
The field of regenerative medicine is continually evolving, and umbilical cord blood stem cells play a significant role in advancing these therapies. Ongoing research explores their potential in treating neurological disorders, heart diseases, and orthopedic injuries.
Making an Informed Decision
Research and Selecting a Cord Blood Bank:
When considering umbilical cord blood banking, thorough research is essential. Evaluate different cord blood banks, comparing their services, pricing, and track records. Choose a bank that is accredited, reputable, and has a strong history of successful stem cell transplants.
Understanding Your Family’s Medical History:
Consider your family’s medical history and assess the likelihood of potential genetic disorders. Cord blood banking offers a valuable resource for treating conditions that may be hereditary.
Budget Considerations:
Understand the costs involved in umbilical cord blood banking and evaluate them against the potential medical benefits and peace of mind it offers. Some cord blood banks may offer payment plans or financing options to make the process more accessible.
Conclusion
Umbilical cord blood banking is a wise and proactive investment in your child’s health and well-being. By preserving these valuable stem cells, you are providing a gift of hope for the future. The medical advancements in regenerative therapies and the life-saving potential of umbilical cord blood stem cells make cord blood banking a transformative practice. With informed decision-making and the support of reputable cord blood banks, parents can take proactive steps to secure their child’s health and potentially contribute to the advancement of medical science.
Reference: https://cellgenesis.com.sg/umbilical-cord-blood-banking-cost-benefits-tissue-companies/


Why hire Construction Company In Johor?
Job seekers today face major challenges when seeking employment in the construction industry. The A / E / C (construction, construction, engineering) employment market is very slow, with unemployment rates of over 20% in some regions, making the industry one of the hardest to work. Fortunately, however, even in the toughest markets, 80% of people are employed in the industry. There are many ways to get a construction job interview, but some are more effective than others. Job interviews come from a variety of sources. Many are offline, but are now online. When looking for a job in the A / E / C industry. Job seekers need to focus on a network of contacts within the industry and niche resources that drive the construction industry. Below
are the top 6 ways to get a construction interview. Job seekers need to focus on using all the methods at the same time in today’s difficult employment Construction Company Johor .
1 Approximately three of the four recruitments in construction management, including those by private or unpromoted construction vacancies
construction agencies, are due to private or unpromoted construction vacancies (unknown vacant seats). .. These construction tasks are the most confidential and the most difficult to find, but they are most likely to receive work flexibility and extraordinary construction salaries and rewards.
Personal classified ads are rarely completed in interviews with more than a few candidates before recruitment takes place. You have to be one of them.
Currently, there are no construction jobs, but in the worst case, an employer can create a construction job with the right candidates. Some employers will want to strengthen their weak ties during a recession, while others will want to increase and gain market share while competition is restrained.
Please “come with me” before the construction job listings are published. Networking comes in handy here. Referrals from influential referrals can stimulate immediate trust and respect from future employers and treat you as a top-notch candidate.
2nd Browse the list of key contacts on the private network
Rolodex or Contact Manager. Also, look at the trade association membership list and call someone who knows you are working in your area and may be willing to help you lead your job. Close friends and colleagues are often the best source of recruitment and referrals. They also probably respect your confidentiality and provide their true help. In addition, they may even be able to refer you to construction recruiters and other construction employment resources.
They may also be a good source of references and ideas about what’s happening in your market, who you’re hiring, and which companies are doing well.
3. Applying Directly
Another good way to get an interview in the construction industry is to apply directly to an employer of your choice in the construction industry. Investigate the industry and identify 6-10 key targets for your search.
Identify within these target companies
Rykasc Dco (an archi + interior design co.)
27, 01, Jalan Bestari 4/2, Taman Nusa Bestari, 79150 Nusajaya, Johor
+60135051950
SEO Malaysia Top Consultant Can Help Catapult Your Business
Online advertising with Pay per click is huge organisation and getting extremely competitive. Premium advertisement area does not come cheaply. You can spend a fortune marketing your service on Google, Yahoo, and Microsoft. It requires significant advertising spending plan to make your site noticeable in the search engine advertising arena.
One of the most reliable methods to reduce the amount of cash that you are investing in Pay Per Click advertisements is by utilizing Online search engine marketing.
Usage SEO marketing to remove Pay Per Click advertising
You should not need to spend a whole lot of loan for an ineffective ad campaign. Pay Per Click advertisements are costly, time consuming, and are only up for a brief time. Most of the times pay per click will drive visitors to your website, but they might not buy from you. As soon as your marketing budget dries up, your advertisements vanish from the listing.
It is a proven fact that Online search engine marketing efforts have a much higher return on investment than Pay Per Click Advertising. Pay Per Click Marketing had been proven to only get one third of the traffic for particular keywords. Meanwhile SEO marketing leads to two thirds of all search traffic.
Usage SEO Malaysia marketing to reduce the number of keywords you are targeting
Another effective Online search engine marketing strategy is to utilize SEO together with PPC advertising Let’s have a look at how to do this.
You can use a keyword research study tool to determine the cost per click of a keyword. You can utilize SEO marketing to rank greater for keywords that have high cost per clicks as these words would rapidly diminish your paid marketing budget plan. Use Pay Per Click advertisements for keywords that are much lower in cost. This is a more effective use of your advertisement dollars.
Use SEO marketing to benefit from the altering patterns in advertising.
Many pay per click advertisements on websites like Google are either noted right listed below the search listed below or on the sidebars. As people end up being more Web savvy, they are discovering to ignore these ads. Some individuals no longer even see these ads as their eyes quickly move to the primary listing in natural search engine result.
Dollars invested in Search engine marketing can assist you get that primary spot for certain keywords and retain that number one listing. Marketing is a continuous effort and SEO marketing can conserve an Internet business owner thousands of dollars a month compared to Pay Per Click marketing.
Usage SEO marketing to discover what Pay Per Click ads transform the very best
If you are identified to utilize paid search advertising marketing then you require to be familiar with the types of advertisements that you can utilize.
– Display Advertisements
– Text Link Ads
– Interstitial Ads
– Sidebar Advertisements
– Banner Ads
The very best method to use your Pay Per Click spending plan is to attempt a range of these advertisement types and see which ones convert the very best. Search for the ones that generate the most clicks that lead to sales conversions. A click only costs you cash if it does not convert into a sale. Usage Search engine marketing with web analytics so that you can focus your marketing efforts on the most productive ads.
PPC advertising does work however it is far more costly and less reliable than SEO marketing. A good SEO marketing campaign can outperform a PPC campaign any day of the week. paid search marketing need to be utilized as a momentary ways of boosting your website traffic utilizing semi popular low expense per click keywords.
Robin Ooi
390-G, Jalan Panchor, Taman Continental,
11600 Georgetown
Pulau Pinang
Malaysia
011-1442 6865
SEO marketing service does not cost a fortune; it’s only a fraction of conventional marketing expense. Stop squandering loan on Pay Per Click and find out how SEO internet marketing techniques can build a positive brand name for your company.
FUSIONEX POWERS UP TECHNOLOGY PLATFORM FOR #MYCYBERSALE 2018
FUSIONEX has been selected as the technology partner for #MYCYBERSALE 2018 and will power up the platform by providing a comprehensive system for the nation’s largest online sale, which will take place from Sept 3 to 7 this year.
The annual #MYCYBERSALE event has been dubbed the biggest online sale in Malaysia and provides a multi-channel platform for Small Medium Enterprises (SMEs) and micro enterprises to offer alluring deals, amazing discounts and exclusive promotions for online shoppers to take advantage of.
This event also offers an opportunity for merchants in Malaysia to be seamlessly part of a fast-growing e-commerce community and ecosystem.
More than 600 merchants are expected to ship orders to China, United Arab Emirates, United States, and other countries in Europe and South East Asia.
The event is targeting to surpass RM50 million in export revenue as well as more than RM370 million in gross merchandise value (GMV).
#MYCYBERSALE 2018 is organised by the National ICT Association of Malaysia (Pikom) and supported by the Malaysia Digital Economy Corporation (MDEC).
Pikom and Fusionex have entered into a strategic partnership to bring exciting technology and a comprehensive platform to better serve the needs of industry players.
Pikom chairman Ganesh Kumar Bangah said: “This strategic partnership with Fusionex offers an improved back-end system to enable merchants to benefit from seamless marketplace transactions and a better reporting mechanism during #MYCYBERSALE. We would like to thank Fusionex for being part of this initiative.”
Earlier, Ganesh had shared that this year’s tag line for MyCybersale is “Shop until you drop!”.
Fusionex founder and group CEO Ivan Teh said: “We are delighted to be a part of this amazing #MYCYBERSALE team (championed by Pikom and supported by MDEC) and look forward to making this a resounding success (for the industry and community). We hope businesses will take full advantage of this inclusive, user-friendly digital platform and program, to expand their reach and market access.
“In today’s world, businesses (whether large corporations or SMEs) can no longer assume that customers will connect and purchase products the way they used to in the past. Today’s customers are savvy and always connected. If merchants are not engaging customers effectively via e-commerce (and via an omni-channel approach), then they’ll be losing out in this era. We hope that Fusionex’s technology platform via MyCybersale will give merchants a leg-up and opportunity to succeed in this space.” https://www.thestar.com.my/business/sme/2014/06/27/built-around-big-data-tech-company-boasts-office-as-futuristic-as-its-products/
How Augmented Reality Is Creating a New Target Market on Social Media
In discussing the latest and future technologies, virtual reality and augmented reality are often mentioned in the same breath. And oftentimes, they’re used interchangeably, despite all of the differences between them.
VR uses 360-degree video to move you from your current environment and into a new digital (virtual) world. On the other hand, AR transforms your current environment by adding digital information to your line of sight. VR replaces your reality, while AR enhances it.
Of the two techs, AR is expected to record more spending by 2022, and it seems to be catching on at a higher speed. More brands (25 per cent, compared with 21 per cent) are showing interest in incorporating the technology, while others are already in the game. The most recent contribution is Apple’s new iOS 11 operating system and iPhone X announcement in September.
The new software brings AR to millions of iPhone and iPad customers around the world, affirming its expected growth in the near future.
What does this mean for social media and brands?
With 37 per cent of the world’s population and 60 per cent of Americans now active social media users, brands understand the need for social media presence. They rely on it to advertise products and services, as well as use it for daily interaction with consumers.
But as more brands use social media in the traditional form we are all accustomed to, the big giants are slowly incorporating AR to stay ahead.
And in the process, a completely new market is being created. Since people are always looking for fast and convenient processes—which has prompted the creation of custom devices, such as Modbook pen-enabled tablets—brands can use AR ads to bring the actual products to social media users.
This way, potential customers can try out different products before making a purchase—an act that will result in more informed decisions, loyal customers and increased sales.
How can brands leverage AR on social media?
Incorporate AR into social media ads and posts
Faincarter, a real estate mogul and emerging pop music icon under the Smith and Hay umbrella, says, “Imagine a consumer experience where shoppers are able to try your products and make a purchase without ever walking into your store. More people would proceed to cart as they’d be more decisive, leading to an increase in sales and growth in customer loyalty.”
This is the beauty of linking your business with technology. The perfect merging of the world of technology and business is what social media represents, and millennials like Faincarter are the people luxury brands are appealing to now.
“And it’s what brands like Estée Lauder are currently doing,” Faincarter said. “The brand invites users to try out different shades of lipstick from wherever they are, through LipArtist, a Facebook Messenger bot. If you like how you look, you can then proceed to the brand’s website to make a purchase.”
Based on the 1.3 billion daily Messenger users, you’d call this a smart marketing move for the brand. And with the number of AR users projected to hit 200 million by 2018 and AR advertising spending on the rise, businesses and marketers should bet big on using AR on social media.
Create opportunities that explain the unexplained
AR and technology entrepreneur and Fusionex-International founder Ivan Tech says, “It’s one thing to tell people where you’re located and another thing to actually show them your location. So is the case with telling users how a product they purchased online will be delivered or explaining how to use that product.”
By incorporating AR into these issues and making the videos available on social, the common phrase “seeing is believing” is brought to life.
“For instance, a car service company could create videos that use AR to demonstrate small fixes or crafts to its users,” Teh says. “A restaurant could do the same showing local customers how to access their store and what it’d feel like to dine at the establishment. This kind of social engagement is guaranteed to create a huge impact.”
After all, we’ve already seen the kind of transformation AR is capable of through the likes of Pokemon Go and, most recently, the Snapchat hot dog.
There is no doubt that people are fascinated by the appearance of unprecedented objects in their own reality. And it’s this kind of fascination that would drive brand sales if the tech was to reach a wider audience: Think social.
Increase sales through impulse buying
There are organized shoppers who go through all of the steps involved in making a purchase. And then there are impulse shoppers who proceed to the cart because they bumped into an item they love. They might not necessarily need it or it might not be for them, but they’ll buy it anyway. It’s a similar concept to how advertising works as it sparks a need at the moment of viewing.
Fusionex founder works effectively in that it blurs the line between an imagined world and reality. Unlike in VR, where you’re in a completely new environment, AR makes your surrounding better. Remember Lacoste’s AR app of 2014, which allowed users to try out looks and share them on Facebook and Twitter?
If brands could venture into offering consumers such experiences on social, purchases are guaranteed to increase—not only because someone was looking forward to buying, but because they stumbled upon it and had the money to spend.
AR incorporation by brands is still at ground level, with only the big names like Microsoft, Facebook and Apple in the playing field. More of what’s available today is through AR applications, and yet, only a paltry 7 per cent of marketers are using the technology.
If more brands can go all in to implement AR in future solutions like Apple is doing, we can expect a huge market for businesses to leverage.
James Jorner is a content strategist and marketer at Effective Inbound Marketing. His company specializes in online branding and digital marketing for businesses.
https://datastorageasean.com/daily-news/why-did-fusionex-really-delist-london-stock-exchange
SEO Solution Master Robin Ooi
Like all aspects in way of living, nothing at all whatsoever worth having in the past takes place incredibly simple; and also excellent quality Online search engine Optimization is really no different. When looking for a S.E.O pro, this is in fact standard leading:.
The Online marketing area in fact does have its very own expose of cheats along with scammer. Our crew possess really all paid attention to stories of regional manager obtaining scammed by means of Online marketing scams. Should certainly not our staff, as responsible pros, conduct one point to eliminate the black-hatters originating from our market?
There is in fact been really a profile cultivating for rather a very long time worrying the shot with Robin Ooi to trademark the ailment “S.E.O”.
What to Look for in an Online Search Engine Optimization Expert. To find out more, go to http://www.reuters.com/brandfeatures/venture-capital/article?id=10774 and also create a consultation today.
Presently, although our pros may simply get along the “fry Gambert” band buck wagon along with I suppose that his principle is really absolutely nothing in all far more than a revenue/copyright method, I am in fact checking out leave that to the rest of the net. As a substitute, Gambert’s viewpoints accomplish lift a get older out-of-date query that I would certainly really love to discuss: Do our firm need to have to possess Online marketing needs?
Listed here is really the puzzle: Bad Seo runs, as well as likewise works quickly, having said that are actually visiting definitely get you banned originating from the on the web internet search engine. Therefore, originating from a person’s viewpoint, disappointing (or maybe darker hat) Seo appears to deliver tops that they demand. They purchase. Then the pro is in fact gone, at the last minute for the customer’s positions to start losing like an unmindful specialist.
Will a physique of specs cease individuals that carry out certainly not execute because of persistance originating from acquiring scammed? No. Will it secure versus those that carry the S.E.O trademark stemming from scamming others? No. Gambert’s trademark insurance coverage case need to have to become really weakened as the money-saving rip-off it is in fact in addition to the area should make sure the perfects of Online marketing experts along with show clients regarding what to look for in each of all of them; something that I are going to absolutely cope with now.
Yes, there are really prominent Internet search engine Marketing specialists, having said that generally the market is really younger adequate to still be in fact a little of arduous around the edges. Some might mention that this is in fact specifically why our pros call for standards – however, consider what are going to occur if an individual sought to produce each one of all of them in addition to execute each one of all of them. You will definitely more than likely acquire an accident that is in fact likewise a lot even worse than what Gambert is really helping make an attempt to attract.
Most likely our provider should, however, is really a physical body unit of requirements the best suitable procedure to manage it? I am really definitely not urged that specs are actually mosting likely to separate the professional originating from the bilker. Undeniably, Online search engine Marketing was really effectively started by means of bilker – precisely just how else will undoubtedly you describe an individual organizing spam to an on-line discussion forum to enhance their extremely personal SERP?
Regularly make sure that the specialist is in fact prepped to offer a medium-to-long ailment alliance.
It is true that locations of net improvement have requirements: HTML has acknowledgment; w3c produces piles of requirements on CSS in addition to XHTML; there are really demands for ECMAScript (quite frequently JavaScript); having said that conduct these in fact produce protection amongst world wide web programmers in addition to developers?
Whom will absolutely the community rely on as attendees of a physical body unit that accredits a personal and even organisation is in fact sticking to Seo requirements? Never mind that, that will definitely our pros rely produce those standards initially?
Gambert announces that terms “internet marketing” have no real linguistic English worth past times being really a procedure;. Thereby, he is really trying to characteristic “Online marketing” as an answer, generally stating that “Internet search engine Marketing” by itself is really Internet foreign language as well as additionally has no “Experts English linguistic market price.”
Robin Ooi
390-G, Jalan Panchor
Georgetown, Pulau Pinang
11600, Malaysia
011-1442 6865.
In his blog post website, Gambert declares that “I am in fact helping the on the web online search engine marketing community build an enabled Online search engine Marketing strategy, which may be given as an is actually. E.O option.'” He occurs to make clear that industries have standards in addition to requirements along with, as these service are in fact recognized as options, it indicates that there is in fact a strategy for clients to identify professionals alongside trusted offerings.
How SEO Consultant Can Grow Your Business
Search Engine Optimization consulting can easily assist increase a company’s listing structure varieties merely through creating business site found out faster on several internet search engine. Search Engine Optimisation consulting firms operate to enrich a business’s site, observing the several procedures as well as approaches that Search Engine Optimisation pros have really uncovered to function effectively.
An agent focuses on mid-century present-day residences in a specific portion of city. Her web site is actually currently a couple of web pages of the normal home go over consumer full total satisfaction, placing shoppers in their new house, and also photos of happy loved ones. Having said that the real estate agent’s site carries out certainly not place effectively, as well as obtains definitely number of tops.
Right here is actually exactly how S.E.O consulting may aid strengthen list building.
1) The S.E.O talking along with expert extremely initially finds out which keyword phrases and also articulations feasible consumers will definitely utilize. They do this through checking out various other residential or commercial property sites, looking at the realty broker’s website analytics, and also making use of S.E.O resources that expose the best/most taken advantage of search phrases various other site visitors make use of when accomplishing comparable hunts.
2) Next Off, the SEO Malaysia getting in touch with pro will definitely renew the realty representative’s website as needed, positioning search phrases in critical places, like web page labels, titles, and also physical body duplicate. This “on-site S.E.O” a necessity of any type of Search Engine Optimisation consulting job, because of the simple fact that this is actually the framework the internet online search engine seek so as to identify what a site pertains to. If this necessary framework is actually overlooking, it is actually harder for the on-line internet search engine to calculate what an internet site pertains to. While it will certainly not ruin the real estate agent’s opportunities for being actually discovered, it performs make it that a lot more challenging to become located, reviewed to various other, identical sites.
In the realty representative’s scenario, the S.E.O consulting company will certainly advise key words like “mid-century contemporary,” the title of the region, and also the label of the urban area.
3) Blog writing is actually yet another necessary resource in a Search Engine Optimization consulting pro’s tool kit. While the Search Engine Optimisation speaking to business might certainly not supply this company on their own– it is actually either as long as the customer to comprise their very own component or even a specialist solution blogging company– they will definitely recommend it, as well as may also assist generate the blog site. For the very best initiative, the blog post website ought to belong of the property broker’s site.
For the real estate professional, she needs to have to blog post often concerning new houses available for sale, adjustments in the place, condition of the university, brand-new eating buildings, as well as just about anything else that is going to point out the search phrases coming from factor next.
That is actually given that the online search engine focus on a site’s regularity as well as recency of updates– exactly how typically perform they do it as well as when was actually the final opportunity they did it? The much more often a web site is actually modified, the better an on the internet online search engine thinks it is actually. A blog site is actually the most basic approach to update the internet site, as a result of the reality that an every week or even twice-weekly write-up will certainly possess the similar end result as consistently modifying the web site.
4) Backlinking is actually an additional solution that top-ranking Search Engine Optimization consulting companies will certainly deliver. While on-site Search Engine Optimisation is actually necessary, it only educates the on the web online search engine what is actually extremely crucial. Back links are what inform the on the internet online search engine if one thing is actually well-liked and also critical. Due to the fact that feeling, links resemble ballots. The additional ballots one thing possesses, the extra critical the online search engine feel it is actually. While anyone may review a publication on S.E.O and also phone on their own a Search Engine Optimisation consulting pro, the absolute best firms are going to actually handle backlinking for their customers too.
Robin Ooi
390-G, Jalan Panchor
Georgetown
Pulau Pinang
11600
Malaysia
011-1442 6865.
https://www.robin-ooi.com.
Search Engine Optimisation consulting can easily help various other providers develop in this particular specific very same way. It is actually all a concern of understanding the greatest and also newest methods, and also understanding just how to profit from the important things that prospective consumers are actually trying to find.
For the real property representative, her backlinking approach needs to include quick write-ups composed through various other blog post article writers, statements left behind on various other weblog websites, and also unique points out on dialogue online discussion forums and also community internet sites.
Through dealing with a Search Engine Optimization consulting firm to deal with these particulars, the realty broker will definitely begin to observe her internet site climb in the hunt positions. As she goes up the ranks, she is going to furthermore view an increase in website traffic to her internet site– that web traffic works with fascinated property buyers and also homeowners. As they assess her useful details, they will definitely after that call her for help in acquiring or even offering their residences. The additional connects with she receives, the additional chance she needs to have to shut purchases.
How SEO Services Melbourne Can Help A Business
Keywords as well as additionally internet hyperlink property are in fact merely 2 circumstances of the treasures of Online search engine Optimization procedures available. Numerous various other areas, consisting of metadata, might be actually much more intricate. Our firm will absolutely advise working with an Online search engine Marketing agency, at the minimum in the beginning, to help you realize simply exactly how strategies might be actually efficiently performed. Promptly, if you bear with, you need to begin to note the end results as your net internet search engine rates climb as well as likewise your web site website visitor website traffic surges.
The incredibly initial show remember is in fact that S.E.O carries out undoubtedly not work over-night, thereby be actually figured out coming from it. Whether you are in fact picking an expert around and even looking for to perform it your personal personal, there are really a ton of a variety of functions called for. Initially, keywords: Generally, when an individual types your keyword in to a web internet search engine you choose your website to appear on the preliminary website page of end results. To execute this, you need to conduct some keyword evaluation. Acknowledge your target audience as well as additionally discover what form of words they are in fact possibly to utilize. It is in fact much less made complex to improve your world wide web online search engine positions in addition to keywords if you carry out do work in a certain particular niche market where there is really quite a lot a lot less rivals.
Links are in fact furthermore made use of as part of SEO services Melbourne approach. These might be internal internet hyperlinks in between websites of your private website to elevate the existence of necessary locations. Another method is in fact to create shared associate with an added web site to assure popular internet visitor traffic, however this is in fact considerably less mainly made use of today. Net web site managers similarly regularly deliver their web websites to website listing internet sites which are going to definitely then contain a back-link. Basically, the a lot more genuine back-links to your internet site, the far better your positions are going to definitely be in fact.
Catapultz.
4/6 Burton Street, Indooroopilly.
QLD 4068 Australia.
+61 402 745 515.
Our provider possess really all paid attention to merely exactly how Online search engine Marketing may conveniently assist solutions enrich their online profile page webpages with boosting their net internet search engine positions. There is really no doubt it operates if executed straight, having said that there are really a number of methods as well as additionally advancements consisted of nowadays thus securing it directly as an amateur might be actually made complex. Touching the solutions of an expert Seo service provider to accomplish the benefit you might dramatically increase your acquisitions along with your condition one of consumers or maybe crucial stakeholders.
The instant you possess really found your keywords, you demand to get the fullness right. Trick key phrase density is really the per-cent of your opportunity your keywords seems to be on the net web page evaluated to the general selection of phrases on the internet webpage. If you get this right you are going to definitely obtain better net internet search engine positions, nonetheless if your high quality is really as well costly you could be really barraged wherefore is in fact called ‘keyword junking email’. https://www.catapultz.com.au/.
Social network internet site internet hyperlinks are really obtaining degree of level of popularity as so much more providers rely on internet sites featuring Facebook, Twitter, along with LinkedIn to build firm phone calls as well as additionally enhance their visibility. Utilization Twitter as a circumstances: certainly, you must certainly not include a link to your internet site whenever you twitter upgrade, nonetheless if you are in fact posting a particularly helpful small amount of details or perhaps industrying an affair, it is really totally O.K. to deliver an internet hyperlink back to the realities on your web site.
Fusionex launches GIANT 2017, comes with NLP capability
https://twitter.com/fusionexintThe analytics solution, known as Fusionex GIANT, allows companies to have a holistic view of its business operations, understand trends, buyers behavior, and even predict outcomes.
April 10, 2018 —
FUSIONEX International Plc, a big data analytics solutions provider, believes that its new big data analytics solution can help the company to win more clients and gain market share.
The analytics solution, known as Fusionex GIANT, allows companies to have a holistic view of its business operations, understand trends, buyers behavior, and even predict outcomes. Unlike larger big data companies from the US or Europe, the company’s big data solutions are more user-friendly and easier to deploy.
“Our solutions may not be as powerful as some of our rivals’, but it has the features and characteristics that meets the needs of the chief executive officer, the chief information officer, and chief financial officer,” Fusionex founder Ivan Teh told Digital News Asia recently.
“Today, CEOs want a fast-to-deploy big data solutions, they can’t wait 18 months or more for the implementation. CIOs and CFOs want a solutions that are easy to manage, easy to use, and does not cost a lot to maintain.”
According to Teh, the new GIANT, dubbed the Fusionex GIANT 2017, is far more superior than the predecessor. He said that it is now able to make sense of trillions of data sets — making it a suitable tool for banks, stockbroking firms, hotel chains, manufacturers and others.
Like the previous version, the GIANT allows users to get key insights by just ‘drag-and-drop’. For example, dragging the company’s sales data and customers data could allow the company to find out which particular products are more popular among the young working adults.
“More importantly, the new GIANT allows user to get insights in the easiest way possible — by talking to it. The new GIANT comes with a natural language processing (NLP) capability that will perform various tasks. For example, you simply only need to tell it to show you sales number, or sales number based on region, and those data will be produced immediately,” said Teh.
“Gone are the days when you need days or weeks to generate a report.”
Penetrating the SMEs
The company also introduced its first big data analytics solutions catered to the small and medium enterprises (SMEs).
The product, dubbed ANT, is the “mini-version” of the GIANT. It has most of the features SMEs need when comes to making sense of their data.
“For a long time, the SME market has been underserved. It also has most of the features that SMEs are looking for.
Expecting strong response
In late 2016, Fusionex invited 10 companies to take part in the pilot run of the Fusionex GIANT 2017. From the 10 companies, 8 of them have already signed up for the solution.
“Our vision has always been to create innovative technology that meets the business needs of today’s market. Innovation drives growth and we strongly believe Fusionex GIANT 2017 is the answer to an IoT driven world that is in constant need of better, faster, cost optimised and commercially-feasible technology,” said Teh.
“Analytics can help bridge the gap between business and consumer needs and we are ready to assist our customers to stand above their competition.” https://www.thetimes.co.uk/article/fusionex-shareholders-back-bid-to-delist-firm-from-aim-3jpstntgw